
When Neuromuscular Disease Affects the Brain
Some children with MD have cognitive or emotional problems, along with physical disabilities
 If you’re the parent of a child with a neuromuscular disease, you’ve probably heard something about learning disabilities, mental retardation or emotional problems that accompany some of the muscular dystrophies and related diseases.
If you’re the parent of a child with a neuromuscular disease, you’ve probably heard something about learning disabilities, mental retardation or emotional problems that accompany some of the muscular dystrophies and related diseases.
But this information is often expressed in vague, general terms, leaving a parent wondering what specifically has gone wrong, whether the child’s school problem is directly related to his neuromuscular disease or not, and — perhaps most important — what can be done to help.
Several neuromuscular diseases can involve cognitive problems. They most commonly occur in Duchenne, Becker, congenital and myotonic muscular dystrophies, and in mitochondrial diseases. Of course, not every child with one of these disorders will have cognitive disabilities, but the risk is higher than average.
Duchenne MD: a cognitive profile
So, let’s say your 10-year-old with Duchenne muscular dystrophy (DMD) has been given a diagnosis of “learning disability.” Let’s say he also seems emotionally distant and increasingly distressed at his inability to keep up physically.
What do you do?
That’s a tough one to sort out, most doctors would say. But there are some clues here.
Neuropsychologist Veronica Hinton, at Columbia University in New York, studies children with DMD and its less severe variant, Becker MD (BMD). She’s compared the scores of boys with DMD and BMD to those of their unaffected siblings on several detailed tests of cognition.
In her studies, Hinton found a clear pattern, what she calls a “DMD cognitive profile.” The children with DMD were almost universally weak in certain cognitive areas that have to do with processing recently heard oral information. In tests that asked them to repeat a string of numbers they’d just heard, they consistently did more poorly than their siblings.
Modern experts believe that about 5 percent of boys with DMD are mentally retarded and that about a third have some degree of mental impairment or learning disability. Because studies have been conducted at different times and in different countries, definitions of these terms haven’t been consistent, and older literature is particularly misleading, sometimes suggesting that as many as 33 percent of boys with DMD are mentally retarded.
Hinton believes that the cognitive problems she’s identified — deficits in verbal short-term memory or phonologic processing (the ability to process and recall sounds just heard) — probably place all children with DMD and BMD at risk for learning disabilities. But she finds that many children with these deficits have high enough general intelligence to compensate for the disorder. Others, with perhaps less well developed compensations, fall into the “learning disabled” category in school.
Hinton compares what happens when a child has DMD and a learning disability to the experience of someone who’s learning a new language and enters a room in which native speakers are conversing. “You pick up a word here and there, but you know you’re not processing things the way you would like to be. You’re able to sort of make sense of the conversation — you’re getting some words and not others and trying to fill in gaps.
“For a lot of these kids, it’s a bit like that.”
Identifying the problem
So, what does she recommend? First of all, identifying the problem, preferably by a thorough neuropsychological evaluation by someone who’s familiar with testing children on detailed tests of cognitive function. (Ask at your MDA clinic for this type of referral.)
Then you can tailor the child’s educational program to his strengths.
Hinton says, “The most important thing that people need to know [about boys with DMD and BMD] is that the majority of cognitive skills are developing properly. Everybody has some things that they’re better in or worse in.
“But when you look at these kids as a group, there is one area [processing of information just heard] where they all do a little more poorly, and it’s consistent across the group. Given that, it suggests that there’s something about the disorder that’s affecting [learning].
“We don’t think it has to do with being treated differently because of the disorder. We think it’s something specific to the disorder, not something that’s reacting to it.”
And what is that “something specific”? It probably has to do with dystrophin, the protein missing in the muscles of boys with DMD and diminished in those of boys with BMD.
Dystrophin is obviously important in muscles, but recent evidence suggests it also has importance in the brain. Most children with DMD and BMD probably don’t have entirely normal brain dystrophin, although there may be differences in the type or amount of the protein in different children.
Learning disabilities don’t seem to be correlated with muscle weakness, and there’s little evidence that they go along with particular types of mutations in the dystrophin gene. So far, as one expert put it, the role of dystrophin in the brain and its relationship to muscle dystrophin has remained somewhat mysterious.
Many roles for dystrophin?
What about this fictional child’s other problems — his emotional distance, moodiness, unhappiness as his muscle weakness begins to separate him from his classmates’ athletic achievements?
Mark Mehler, a neurologist and neuroscientist at Albert Einstein College of Medicine in New York, has received MDA funding to study brain involvement in DMD and BMD.
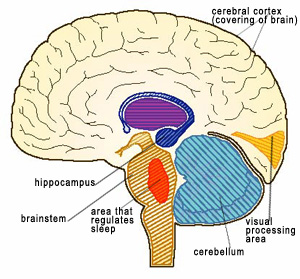
Mehler says dystrophin is normally located in specific areas of the brain — notably the hippocampus, cerebellum and cerebral cortex, particularly the part toward the front of the head. These are the areas that have the most to do with memory, attention, planning of movement and thinking, Mehler says, noting that “these functions appear to be disproportionately impaired” in boys with DMD.
“It turns out that there are different forms of dystrophin in the brain, and the way it’s arrayed in the brain during development is a thousand times more complicated than the way it is in muscle. That chapter is just beginning to be written,” Mehler says.
And he’s among those writing the chapter. Emotional manifestations are part of the dystrophin deficiency in the brain, Mehler speculates.
“Things that involve the emotions can be ‘off,’“ he notes. “A child may appear not engaged or involved — or may be overly so. There can be some ‘disconnect’ between the individual and his environment. The usual stimuli [signals] in the environment that will provoke somebody to do something seem to get crossed, not processed properly, so that the child doesn’t appear to be connected with the person they’re interacting with.
“Conversely, the child can know no boundaries.” Sometimes, young children with DMD will jump on a stranger’s lap or play with a stranger’s face, Mehler has found.
“A large part of the [cognitive] disorder in Duchenne and Becker is due to biology and isn’t due to things related to the disability per se,” Mehler says. However, he cautions, the reactions of the child and family to the devastating effects of having DMD can certainly compound the problem.
Parents, he finds, are often relieved, rather than distressed, to find that their child’s cognitive or emotional problems are part of his neuromuscular disease and not something separate.
Is it really an attention deficit?
As for treatment, doctors admit there isn’t much. These cognitive disorders fall on the borders between the territories of the neurologist, the psychologist and the education specialist. The important thing is not to fall through the cracks.
Some doctors prescribe medications such as Ritalin for boys with DMD who appear to have attention difficulties.
Veronica Hinton cautions that a diagnosis of attention deficit must be made precisely and that sometimes impaired verbal memory can be mistaken for an attention deficit disorder. The two, she says, are completely different.
“Before anyone goes directly to Ritalin, they should make sure that the problem is not specifically a language-processing disorder,” Hinton cautions. “But if Ritalin is effective, more power to them.”
Mehler recommends getting as good a diagnosis as possible and then carefully choosing and monitoring medications, if they’re used.
“I’m somebody who doesn’t believe in overmedicating in any situation,” he says, “But I also believe that there are conditions in which medication is really the better way or a way that should be used in conjunction with other, behavioral modalities [approaches].”
Congenital MDs: brain abnormalities
Some of the most serious brain effects in neuromuscular diseases are found in congenital muscular dystrophies, a group of diseases still undergoing description and genetic classification.
Three rare forms of CMD are Fukuyama CMD, found almost exclusively in people of Japanese heritage; muscle-eye-brain disease; and Walker-Warburg syndrome. In these, brain cells fail to locate to the right place during the development of the baby in the uterus. Severe mental retardation and vision abnormalities are common in these, as are seizures, the result of abnormal nerve impulses traveling through the brain.
The other forms of CMD are classified into two general categories, based on how much of the protein merosin is present in muscle cells (determined by a muscle biopsy). These are merosin-positive CMD and merosin-deficient or merosin-negative CMD.
Parents are sometimes told that merosin-negative CMD puts children at risk for cognitive difficulties and that merosin-positive CMD generally doesn’t. But, when it comes to talking about brains, the “merosin status” may not be as relevant as other factors.
Ronald Cohn, a physician in training in pediatrics and genetics at Johns Hopkins University in Baltimore, says there may be better ways than merosin measures to predict whether a child will or won’t have major cognitive disabilities.
Those measures include an MRI, or magnetic resonance imaging, scan; and whether or not the child has seizures (sometimes called epilepsy).
Some children with merosin-negative CMD have “white matter abnormalities” that are visible on brain MRI scans, Cohn says. These probably reflect a problem with myelin, a substance that coats nerve fibers. Surprisingly, these abnormalities don’t seem to indicate brain function problems, even though physicians expected big problems when they first began to see these on high-tech scans some 15 years ago.
“It’s quite amazing to see that, although there are substantial visible abnormalities in the brain, such as all these white matter changes, in terms of cognitive function, most of the kids do fairly well.” This seems especially true in those with merosin-negative CMD, Cohn says.
But in children with merosin-negative CMD whose MRI scans show structural brain abnormalities, there’s less reason to be optimistic about cognitive development. Children with, for example, abnormally small brains or cerebellums are at risk for a range of problems, from learning disabilities and reading difficulties to severe mental retardation.
“These kids have difficulties,” he says. “But the difficulties have a huge range.” So far, only small studies have been done in this area.
Children with merosin-negative CMD who have seizures are also at risk for learning problems, especially if the seizures are hard to control with medication. Cohn doesn’t think it’s the primary brain abnormality that causes the cognitive deficits in some of the children, but rather the damage from the seizures themselves, over time.
Many children with CMD show abnormalities in tests measuring the brain’s responses to visual patterns, but that doesn’t mean they’ll have visual difficulties, Cohn explains. He recommends yearly or twice-yearly vision and hearing tests in case there’s something treatable that can be caught. As children with CMD live longer, largely because of better respiratory care, he predicts that sensory deficits in vision and hearing may be detected more often.
The vision problems appear to be in the brain, not the eyes, so Cohn believes the best treatment may be special vision training, rather than conventional approaches, such as eyeglasses.
Recent studies have implicated the protein alpha-dystroglycan in the CMDs that affect the brain. This protein may be a vital link that allows cells to signal each other. The findings have also tentatively suggested that alpha-dystroglycan may be the real culprit in the cognitive problems associated with DMD and BMD , because when the dystrophin protein is missing (at least in muscle cells), so is alpha-dystroglycan. Without dystrophin, alpha-dystroglycan apparently can’t insert itself into the right location in the cell.
Myotonic dystrophy: high risk for body and brain
Myotonic muscular dystrophy (MMD) is a complex disease that affects many systems in the body and brain. In type 1 MMD, the genetic defect can vary in size, and in general, the bigger the genetic defect, the sooner symptoms develop and the worse they are. (Type 2, identified last year, hasn’t been nearly as well studied.)
The most serious form of type 1 MMD is congenital-onset MMD, in which symptoms are present at or near birth. Only slightly less serious is childhood-onset type 1 MMD. When the disease begins in adolescence or adulthood, the symptoms are different and usually less severe, particularly with respect to the brain.
Children with congenital- or childhood-onset MMD often show mental retardation, as well as severe facial weakness and speech abnormalities. Sometimes, especially when a child is very young, it can be hard to figure out which of those factors are the most important in his or her apparent inability to speak and interact with the environment.
Neurologist Charles Thornton, who co-directs the MDA clinic at the University of Rochester (N.Y.) Medical Center, where he also conducts MDA-backed research in MMD, sees a clear distinction between early-onset and late-onset MMD.
“People with congenital myotonic dystrophy have unequivocal, major problems with mental functioning,” he says. “But in adult-onset myotonic dystrophy, the situation is much less consistent.”
Thornton says that in those with early-onset MMD “more than 75 percent have problems with mental functioning that are a significant obstacle with schooling or gaining independence.”
At one time, many experts believed that respiratory stress during the birth process was responsible for a large part of the mental retardation in congenital MMD. This factor is no longer widely believed to be the major cause of the problem.
Children with early-onset MMD often show brains that are smaller than normal and brains in which cells have ended up in the wrong place throughout the cortex.
“The problems in congenital myotonic dystrophy might be qualitatively different from the ones in adult-onset myotonic dystrophy in terms of the type of abnormality occurring inside cells,” Thornton says. “It’s still very mysterious, but people have found things like enlargement of the cerebral ventricles [the fluid-filled spaces of the brain], and there may be some problems with how the brain is formed in the first place.”
In later-onset type 1 MMD (from adolescence on), the problems are far less clear. An adolescent with this type of MMD may be overly sleepy during the day or have no initiative.
Studies have found that the brains of people with adult-onset MMD don’t look like those of the childhood-onset patients, but they have some unusual characteristics. Notably, they can show some loss of cells in the brainstem, where areas that regulate sleep and wakefulness are located, and the thalamus, where sensations and perceptions are received and sent on their way to other brain areas.
They also show some tangled nerve fibers, mainly in the brainstem and areas in the middle of the brain where aspects of learning and emotion are processed.
Very recent studies have suggested that unusual forms of a protein called tau in the brains of those with MMD may underlie at least some of the characteristic cognitive profile seen in adults with this disease and may also have something to do with the mental retardation seen in the early-onset form of the disease.
Medications such as methylphenidate (brand name Ritalin) and modafinil (Provigil) can sometimes help people overcome excessive sleepiness during the day in MMD, Thornton has found.
But some people with MMD are sleepy because of impaired respiratory function (not getting enough air and oxygen into their lungs) and poor circulation from less than adequate heart function. These conditions — more characteristic of late-onset MMD than the congenital form — should be checked for and, when necessary, treated. Assisted mechanical ventilation by mask during the night can help improve air exchange, and devices such as pacemakers are sometimes necessary to normalize an irregular heartbeat.
Thornton emphasizes that “in people with adult-onset myotonic dystrophy, the situation [for cognitive functioning] is much less consistent than in those with congenital-onset disease. It’s important not to stigmatize the disease, because we have met many high-functioning individuals with myotonic dystrophy.”
What few observations have been made in type 2 MMD have shown the cognitive problems, if there are any, to be “more mild and less consistent” than in the type 1 forms, Thornton notes.
Mitochondrial diseases: damage to the brain
Of all the neuromuscular diseases covered in MDA’s program, those that have to do with the mitochondria — the tiny energy-producing units tucked inside human and animal cells — are perhaps the most mysterious, confusing and challenging for physicians and families.
All cells and the tissues in which they’re located require energy to function, but some tissues — such as the brain and muscles — require more energy than others. That’s probably why defects in mitochondrial function hit these areas hard.
There are several types of mitochondrial diseases, and they all have different characteristics. What’s even more confusing is that even when a mitochondrial disease runs in a family, various family members can have different symptoms or degrees of severity, even though their mitochondrial flaw may be the same.
Neuromuscular disease specialist Tim Miller at Arizona Health Sciences Center in Tucson says it isn’t so much the mitochondrial defect itself that makes the difference in cognitive functioning. Instead, as with the congenital muscular dystrophies, it’s the presence or absence of severe seizures, as well as two other aspects of mitochondrial disease — strokes and high levels of lactic acid in the blood.
“Seizures are a major factor,” Miller says. “For kids with underlying mitochondrial changes, you have to worry, because seizures can damage things even worse.”
Fortunately, Miller says, seizures can often be adequately controlled with medication. But these medications can themselves cause some side effects, which can include sleepiness, confusion, memory problems and trouble with vision. The benefits and side effects have to be carefully weighed by the doctor and parents and the dose meticulously monitored.
Strokes or “strokelike episodes” occur in some children with mitochondrial diseases. A “stroke” is the term for an interruption of blood supply to the brain, with resulting brain damage, either temporary or permanent. Strokes can be caused by either abnormal bleeding in the brain or an obstruction to blood flow in the brain.
“There are probably changes in the brain’s blood vessels,” Miller says. “We know that mitochondrial dysfunction can affect blood vessels.” (Other experts say strokelike episodes may sometimes be seizure-related.) Unfortunately, there’s little that can be done to prevent or control these episodes.
When mitochondria don’t produce energy for cells in the usual way, energy-producing pathways are altered, leading ultimately to the buildup of lactic acid. When enough of this chemical gets into the blood, it changes the blood’s acidity level, which leads to a host of unwelcome changes in body chemistry. This lactic acidosis isn’t good for the brain, causing a variety of cognitive symptoms.
“The body maintains a very strict level of acids and bases,” Miller says. “Any time that level is affected, it can affect thinking.”
Miller says a medication called lactulose (brand names Constilac, Chronulac and others) can sometimes be used effectively to draw off some of the acid into the intestines, but that the best approach may be to try to prevent lactic acid buildup from occurring in the first place.
Making sure the child’s respiratory function is adequate, preventing or promptly treating infections, and maintaining good nutrition can all help prevent lactic acidosis, Miller says.
“When kids are challenged with something like an infection, that may make it more difficult for them to stay in [metabolic] balance,” he says. Parents have to be on the lookout for signs of infection and for cognitive symptoms that suggest lactic acid may be building up. Diminished concentration, diminished talking, confusion and irritability are among those symptoms.
The brain’s vision-processing cells, as well as the retina at the back of the eye and the muscles that control eye movements, can all be affected in mitochon-drial diseases, so vision can be a problem.
Vision therapy may be helpful, as can assistive technology such as adapted computer screens and computer-operating devices.
Hearing can also be affected, and some children need hearing aids and/or devices to help them communicate.
Children with mitochondrial diseases and their families often need referrals to hearing and speech specialists, vision specialists, respiratory doctors and therapists, educational specialists, and social workers or counselors. (Ask about these specialists at your MDA clinic and through the public school system in your area.)
GLOSSARY
attention deficit disorder: a neurobiological disorder that interferes with the ability to attend to tasks in an age-appropriate way and to sustain attention and concentration
attention deficit hyperactivity disorder: above, combined with age-inappropriate high activity levels and overly impulsive and disruptive behavior; may be masked in children with severe mobility impairment
cognition: the mental processes by which knowledge is acquired, including perception, reasoning, judgment, intuition and memory
cognitive disability: a problem with cognition
Individualized Education Plan (IEP): a statement for each public school student with a disability that includes information about the child’s educational performance and measurable annual goals, plus program modifications, related services and supplementary aids to be provided to the child. IEPs are guaranteed by the Individuals with Disabilities Education Act (IDEA) of 1997.
learning disability: a disorder that affects the ability either to interpret what’s seen and heard or to link information from different parts of the brain
mental retardation: below-normal intellectual function that has its cause or onset early in life, with impaired learning, social adjustment and maturation; tests to assess it are controversial.
seizures (epilepsy):a recurrent disorder of brain function marked by sudden, brief attacks of altered consciousness, movement or sensory phenomena; symptoms range from slight alteration in consciousness to dramatic loss of consciousness, falling and/or involuntary muscle contractions.
MDA Resource Center: We’re Here For You
Our trained specialists are here to provide one-on-one support for every part of your journey. Send a message below or call us at 1-833-ASK-MDA1 (1-833-275-6321). If you live outside the U.S., we may be able to connect you to muscular dystrophy groups in your area, but MDA programs are only available in the U.S.
Request Information