
Strategies to Improve FA-Affected Speech
Anne Wallace, speech-language pathologist and clinical associate professor in the Department of Communication Sciences & Disorders, University of Iowa in Iowa City, has been at that facility for 20 years. During that time, she’s had a long-standing relationship with the pediatric specialty clinics, including the MDA clinic directed by child neurologist Katherine Mathews, and has worked with many children and young adults with Friedreich's ataxia (FA).
Q: What are the speech-related issues in FA?
A: The main problem is dysarthria, which means a motor speech disorder, not a cognitive speech disorder. Cognition is generally intact in Friedreich’s ataxia.
Dysarthria is caused by things such as muscle paralysis or weakness of the muscles related to speech production or inability to coordinate these muscles. Those are the muscles of the lips, tongue and throat, and also the respiratory muscles that push air over the vocal cords. You have to have respiratory muscles working together to create air flow to make your vocal folds work.
In Friedreich’s ataxia, there are breakdowns in the system of speech production. There can be varied problems that result, such as speech that is slurred or slow, or problems with the pitch or loudness or rhythm of the speech.
Friedreich’s ataxia speech is typically pretty slow and deliberate. The syllables are produced pretty much with equal stress on each word. For example, if I’m saying “banana peel,” I’m not saying ba-na-na-peel, with the same stress on every syllable. Someone with Friedreich’s might, however, do that.
There’s less contrast between the stressed and unstressed syllables, so it’s hard to tell, for instance, whether someone is saying “OB-ject” or “ob-JECT,” which are two different things.
The underlying problem with ataxia in general has to do with cerebellar damage. The cerebellum is what controls coordination. The cerebellum controls a lot of the coordination aspects related to speech, as well as to other things, such as walking.
The earlier the onset of the disease, the worse the problems tend to be. For most people with Friedreich’s, the speech problems occur in adulthood, and the onset is gradual. They don’t happen overnight. The problems develop over time, so people have a chance to adapt to them.
Q: Can you talk about some of the specific problems and your approaches to treating them?
A: An average person can say so many words on a breath, and then they automatically breathe at a certain time, usually at normal phrase boundaries. They’ll breathe at the end of a thought or a sentence, not in the middle.
But if all your speech is slow because of muscle coordination problems, you still can only say so many syllables per breath. If your syllables are twice as long, you can only say half as many things. It takes the person with Friedreich’s more breath and more work to say something than it does the average person. For many people, that’s frustrating.
Sometimes in Friedreich’s there’s a voicing problem, where the person’s voice is coming in and out. There can be a problem with a sudden, really loud voice in the middle of a syllable. It’s related to coordination. When you make a syllable louder, you actually use more air. When you use more air, you have even less breath for finishing the rest of what you’re trying to say.
They can learn to regulate these aspects of speech, which are related to control of air flow. For instance, you can work on multisyllabic words, like “computer” or “Episcopal.” One strategy is called backward building. You take a word like “Episcopal,” and you say “pull.” You build it from the back all the way forward. Eventually you get the rhythm of what you need to say.
Then you play around with the stress. We work a lot on making the stresses come out on certain words, practicing phrases such as “I SEE a ball”; “I see A ball”; and “I see a BALL.”
Another problem in Friedreich’s is that consonant precision is not there. [Consonants are sounds that require complete or partial closure of a part of the vocal tract.] A common thing is not putting the final consonant on a word, so that “hat” becomes “ha.”
I work with patients on trying to make more precise sounds, to try to make the consonants better. I work on words that have final consonants, particularly ones that have more air pressure, what we call plosive sounds, like t, d, k and g.
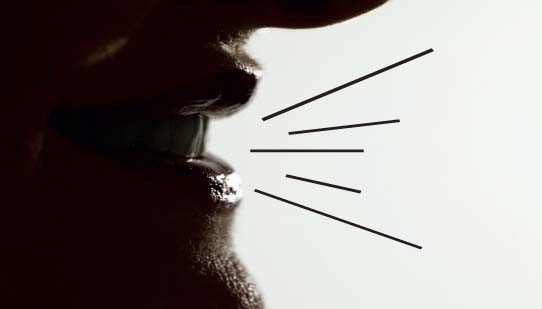
You have to show a person how they need to do that. Sometimes you can use a tactile cue, such as a hand in front of their face. If you were to do that, and say, “hat” with a lot of force, you can feel it on your hand. We also use things like mirrors, which will fog up when you say “hat” forcefully. These techniques add precision to what they say.
What you trade off in order to be able to produce those consonants and improve breath control is that it reduces the rate of speech. But it’s better to slightly reduce your rate than to have all your consonants missing or have the stresses wrong.
Of course, the underlying neuromuscular system is the same, but we don’t tax it as much if we reduce the speed.
Q: Do you have to adjust techniques to disease progression?
A: Yes, you do. Some people continue to be successful with minimal prompting. They learn how to adapt. But there are some people who require some augmentative systems [such as talking computers] at some point. Certainly not everybody.
I don’t recommend augmentative devices lightly. You can have a high-tech system, such as a voice output device, but the more high-tech it gets, the more transporting the device becomes a problem. If you’re using a wheelchair, and the device is connected to your wheelchair, then it’s there for you, and it might be easily accessible. But what do you do when you’re not in your chair? How do you communicate then? Do you have to always be in your chair to communicate?
Lots of times, families that have younger kids will say, “Let’s get the best kind of computer.” But here’s the deal: You’ve got to haul it. The child has to haul it, and maybe they have other motor problems, making that prohibitive. Or maybe the battery won’t hold a charge. There are a lot of issues.
I try to figure out what their communication demands are and match that to what their abilities are and supplement them as needed with an augmentative system or an assistive system, whether that be low-tech or high-tech. I’m not an augmentative technology expert, but I do know that it’s not always an easy solution, and many times we work for years trying to find an augmentative system that works best for a person’s communication needs.
The bottom line is: Can they communicate what they want with their family or in a work setting in a way so that they’re not frustrated by it?
Q: Can most people achieve that?
A: I think so. At least a lot of people can. However, I do think the communication deficit in Friedreich’s does pose a lot of problems. Sometimes, people perceive Friedreich’s patients as not being intelligent because of the slow, labored speech. It makes it seem like their cognitive skills are not intact. That’s far from the truth, but this is a frustration.
Unfortunately, sometimes there’s just less interest in interacting, because speech is a lot of work. I always hate to see that happen.
Another issue is that it’s hard to listen to this speech. If you’re the patient’s partner or parent, there can be an urge, when you see how much work the speech is, to fill in, to jump ahead. But it can be devastating to somebody that’s trying to communicate some information or a thought or an idea. It defeats somebody’s purpose in trying to communicate.
We try to work with families. As long as it takes the person to say something, we tell them to try to patiently wait it out. If the person is trying, you want to support that. It doesn’t help as much as you think to fill in for them. But it can be hard for families to be good listeners.
Q: Is it best for someone with FA to start a speech program as soon as they begin to develop problems, or does that matter?
A: We see patients at different points all the way along. I’m big on intervening early, though, so that people know what’s available. I think what helps in the very beginning is to alert people, to tell them that these are the problems that are probably going to arise, and these are the resources that are available to you.
Then, if they see that their speech is deteriorating — for instance, if people are asking “what?” more often than not, or if they’re recognizing that speech is really laborious — they know there are things they can do to address the problem.
Some early compensatory strategies could be developed that would save them effort and worry, as opposed to waiting until they’re too frustrated to talk.
The entire In Focus: Friedreich’s Ataxia report, can be downloaded from the Friedreich's ataxia disease page.
MDA Resource Center: We’re Here For You
Our trained specialists are here to provide one-on-one support for every part of your journey. Send a message below or call us at 1-833-ASK-MDA1 (1-833-275-6321). If you live outside the U.S., we may be able to connect you to muscular dystrophy groups in your area, but MDA programs are only available in the U.S.
Request Information