
Not Just Horsing Around

Reaping the benefits of therapeutic riding and hippotherapy
It’s good to be back in the saddle.
I thought my horseback-riding days were over due to the progression of Friedreich’s ataxia, until I found Therapeutic Riding of Tucson (TROT) in Arizona.
I’m finishing up my second 12-week session at TROT, and I’ve noticed that — even with having a neuromuscular disease at age 33 — I’ve experienced many benefits from therapeutic riding.
Although many of the riders at TROT are children with cognitive disabilities, I’d like to make other adults with neuromuscular diseases aware of the physical and emotional benefits to be found in therapeutic riding and hippotherapy.
Therapeutic riding vs. hippotherapy
A lot of people think therapeutic riding and hippotherapy are the same, but there are some major differences between the two.
The main goal of therapeutic riding is to teach individuals with disabilities to ride horseback. As they continue to ride, most riders are able to ride better and more independently.
Some therapeutic riding centers also offer hippotherapy, which is always conducted by a licensed physical or occupational therapist (PT or OT).
Hippotherapy is a treatment strategy that uses the horse as a tool to work on specific goals, such as improving balance, coordination, head control and fine motor skills, says Susan March, program manager and PT for Bit-By-Bit Therapeutic Riding Center in Parkland, Fla.
 “Some individuals need the specialty of the therapist because their bodies are not capable of just taking a regular riding lesson,” says Sharon Gilbert, office manager for the American Hippotherapy Association (AHA), based in Fort Collins, Colo. The therapist’s goal is to help individuals to advance out of hippotherapy and into regular therapeutic riding lessons.
“Some individuals need the specialty of the therapist because their bodies are not capable of just taking a regular riding lesson,” says Sharon Gilbert, office manager for the American Hippotherapy Association (AHA), based in Fort Collins, Colo. The therapist’s goal is to help individuals to advance out of hippotherapy and into regular therapeutic riding lessons.
To ensure the highest standards possible and the safety of the riders, a therapeutic riding center and its instructors should be certified by the Professional Association of Therapeutic Horsemanship International, or PATH Intl. (formerly the North American Riding for the Handicapped Association).
If hippotherapy is being done, it’s important to work with an OT or PT who’s specifically trained in hippotherapy and registered with AHA. In addition, therapists should be certified by PATH Intl., or else accompanied by a certified staff member. Some therapists go above and beyond and become hippotherapy clinical specialists, a designation showing advanced knowledge in hippotherapy.
Therapeutic riding sessions can take place privately or in groups, but hippotherapy sessions are always private, Gilbert says.
Both therapeutic riding and hippotherapy are conducted inside an arena, around the center’s property or out on the trails. Also in both, riders with more experience may weave through barrels or cones, or step over ground poles.
Therapeutic riding costs around $40-$75 for a private session and $30-$75 for a group session. Full or partial scholarships often are available; ask the riding center for more information.
Hippotherapy costs around $80-$115 per session, but some health insurance providers will cover hippotherapy either fully or partially. In some states, such as Florida, Medicaid will cover the bill for hippotherapy. Scholarships also may be available.
Before the ride
Before starting therapeutic riding, the first step is to have a physician complete a medical release form. Next, riders must be evaluated by a therapeutic riding instructor, who tests strength, balance and ability to sit on the horse.
Instructors need to determine how much assistance riders will need while riding and what they can do independently. Next is a test ride for further evaluation.
Before starting hippotherapy, some states and certain insurance providers require a prescription from a physician. Even if a prescription isn’t required, the physician still needs to complete a medical release form.
Hippotherapy requires a more in-depth evaluation, in which therapists assess each individual’s strengths and weaknesses and develop a specific treatment plan, says March, who’s registered with AHA and has been with Bit-By-Bit Therapeutic Riding Center for 10 years. From that information, therapists develop exercises, she says.
Special horses, saddles and reins
In both therapeutic riding and hippotherapy, the horses have been carefully selected for this type of work.
“I’m usually looking for a horse that has a very quiet nature — sound and not spooky,” says Mary Vardi, a PATH Intl.-certified therapeutic riding instructor for TROT who’s been involved in therapeutic riding for more than 20 years.
“He needs to move well, meaning that he has a good walk and a good trot, and he needs to be responsive — but not too responsive.” Vardi usually chooses horses between the ages of 8 and 15 for the program.
Therapeutic riding instructors match horses with individuals depending on the horse’s size and width, its temperament and the pace at which it walks and trots.
 The type of saddle used depends on the amount of support riders need. For example, a western saddle gives more support than an English saddle, which requires more control and balance from the rider.
The type of saddle used depends on the amount of support riders need. For example, a western saddle gives more support than an English saddle, which requires more control and balance from the rider.
For those who need even more support, a variety of adapted saddles are available at some therapeutic riding centers says Cheryl West, program manager and PATH Intl.-certified head instructor for the American Therapeutic Riding Center in Sand Springs, Okla.
Adapted saddles may have handle bars on the front or high backs to help stabilize riders with severe trunk control issues, West says.
Sometimes riders will use a type of surcingle, which is a leather or nylon harness that runs from in front of the rider to the horse’s rib cage. Usually a surcingle has one or two handles on top and rests on a western saddle pad.
For hippotherapy, therapists are most likely to use a surcingle and a western pad to allow the rider more movement.
Some therapeutic riding centers also offer a variety of reins. Sometimes looped reins help riders who have difficulty holding the reins, because they can slip their fingers through the loops.
Once the horse is ready to go, it’s led to the mounting ramp where the rider is waiting. An overhead lift hoists the rider onto the saddle or surcingle, where he or she is centered and the stirrups are adjusted.
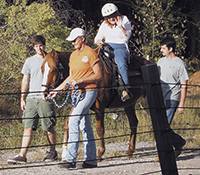
Depending on the disability and the amount of support needed, sessions sometimes feature a small group of participants: the rider, the specially chosen horse, the therapeutic riding instructor or therapist, the horse leader and two side walkers, who are usually volunteers and who walk alongside the horse offering support to the rider.
Emotional benefits
 Both therapeutic riding and hippotherapy are fun ways to spend time outdoors. Since therapeutic riding can take place in group sessions, it also can be a very social activity.
Both therapeutic riding and hippotherapy are fun ways to spend time outdoors. Since therapeutic riding can take place in group sessions, it also can be a very social activity.
For therapeutic riders, mastering the skills needed to control the horse can be excellent for self-esteem and a sense of empowerment. Therapeutic riders and hippotherapy clients often gain confidence as they see themselves improving with each session.
“I’m able to feel more comfortable on the horse and not so scared that I’m going to fall off,” says Camille Levy of Tampa, Fla., who has myotonic muscular dystrophy and uses both a power and manual wheelchair.
Levy, 49, has been riding with Bakas Equestrian Center in Tampa for three months. “It’s helping me to learn how to turn the horse around the poles, which I couldn’t do before. It’s making me happier and that’s what’s important to me.”
Levy says she’s looking forward to winning ribbons for barrel racing in the Special Olympics equestrian competitions.
Hippotherapy is so valuable to Trey Lovell, 23, of Perryville, Ark., that once a week for the past three years he has traveled three hours to Beyond Boundaries in Ward, Ark. Lovell, who has Duchenne muscular dystrophy and uses a power wheelchair, says he really looks forward to spending time with his horse, Comanche.
Physical benefits
Therapeutic riding and hippotherapy confer many physical benefits, and the horse doesn’t even have to be moving for some of these benefits to occur. Just sitting on the horse stretches the adductor muscles of the thighs, says West, who’s been instructing with the American Therapeutic Riding Center for five years. She sometimes has riders with really tight muscles start off on a narrow horse and gradually work their way up to wider and wider horses.
However, the horse’s movement is responsible for the majority of the physical benefits.
“Many times the horse does most of the work,” says West. “Just the motion of the horse will work the majority of the muscles in the rider’s body, including major muscle groups in the legs, arms, buttocks, torso and neck.”
Riders are encouraged to maintain an upright posture against the movement of the horse, a task that stretches their stomach and back muscles. Because the horse’s movements constantly throw the rider off balance, the rider’s muscles are required to contract in order to rebalance, she says.
 Over time, many riders need less trunk support from side walkers and some become more independent while riding.
Over time, many riders need less trunk support from side walkers and some become more independent while riding.
“I have seen kids who are riding without side walkers, who have been doing it for a long time and who are doing really well, and I know that I’ll get that way, too,” says Levy, who already has gained better balance in the three months she’s been riding.
When she first began, Levy supported herself with the saddle horn by “hanging on for dear life.” Now she can hold the reins in one hand and put her other hand in her lap.
Alicia Hammerle,Trey Lovell’s OT at Beyond Boundaries, says she challenges her clients’ balance by changing the horse’s direction or changing the position of the rider on the horse. This shifts the rider’s balance to one side or the other so that they have to use their trunk muscles in order to sit up straight.
“That can help increase their trunk control, so that whenever they’re not on the horse, they’re able to balance better for functional activities such as reaching for a glass on the table or sitting up straight while brushing their teeth,” says Hammerle, who is registered with the AHA and certified by PATH Intl.
As part of his balance exercises, Lovell weaves Comanche through cones and does figure-8s in the arena. He also works on holding the reins, which helps improve dexterity.
“I’ve noticed a significant improvement with Trey,” says Hammerle. “Not long after riding with us he was able to sit up on his own for a short time on his bed, which he wasn’t able to do before he started riding.”
Her advice for those who’ve been participating in hippotherapy, but who can’t participate any longer for one reason or another, is to continue working with a therapist in a clinical setting in order to advance any functional gains they may have made.
Finding a facility
To find a therapeutic riding center, call PATH Intl. at (800) 369-7433, or visit pathintl.org and click on “Find a Center” (select “Therapeutic Riding” or “Hippotherapy”).
Or, contact the American Hippotheray Association at (877) 851-4592; online, click on “Hippotherapy” and choose either “Find a Therapist” or “Find a Facility”.
Happy trails
I’ve enjoyed my experience with TROT and hope to continue riding for as long as possible. Not only does therapeutic riding bring back sentimental memories of my dad and me horseback riding together, but I’m getting stronger both on and off the horse.
More Fun with Horses: Therapeutic Carriage Driving
 Driving a horse-drawn wheelchair-accessible cart or carriage is a popular sport for those who prefer (or need) to control the horse while sitting either in their wheelchair or on the carriage seat. The goal for therapeutic driving students is to learn to guide the horse and carriage by using the reins and their voice.
Driving a horse-drawn wheelchair-accessible cart or carriage is a popular sport for those who prefer (or need) to control the horse while sitting either in their wheelchair or on the carriage seat. The goal for therapeutic driving students is to learn to guide the horse and carriage by using the reins and their voice.
“It’s a two-dimensional sort of movement as opposed to the three-dimensional experience of riding,” explains Bonnie MacCurdy of the National Center for Equine Facilitated Therapy in Woodside, Calif. “A person can be working on goals of flexibility, strength, posture and range of motion while learning a new and exciting skill.”
Sometimes the reins have to be adapted in order to be used by driving students. Rein adaptions can be purchased by therapeutic riding centers, but some driving instructors, such as MacCurdy, prefer to make their own.
For example, for drivers who only can use one hand, MacCurdy made a bar to connect the reins for steering with one hand. She also has fashioned loops in the reins so that driving students with a weak grip can hold the reins easier.
Carriage driving instructors also hold a set of reins and can assist as much or as little as students need, says MacCurdy, who’s pursuing her therapeutic riding and driving certification with PATH Intl. Three to five volunteers usually assist with a driving session.
Only a select group of PATH Intl.-affiliated therapeutic riding centers offer therapeutic driving. They’re listed on the PATH Intl. website (select “Driving” under “Find a Center”), or call PATH Intl. at (800) 369-7433.
Therapeutic driving usually costs around $50 per session, but scholarships may be available to make it more affordable; ask at the riding center for more information.
MDA Resource Center: We’re Here For You
Our trained specialists are here to provide one-on-one support for every part of your journey. Send a message below or call us at 1-833-ASK-MDA1 (1-833-275-6321). If you live outside the U.S., we may be able to connect you to muscular dystrophy groups in your area, but MDA programs are only available in the U.S.
Request Information