Limb-Girdle Muscular Dystrophy (LGMD)
Limb-Girdle Muscular Dystrophy (LGMD)
What is limb-girdle muscular dystrophy?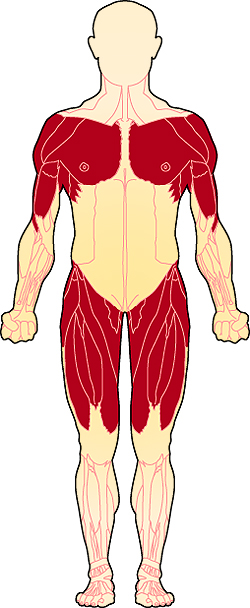
Limb-girdle muscular dystrophy (LGMD) is a diverse group of disorders with many subtypes categorized by disease gene and inheritance. LGMD usually manifests in the proximal muscles around the hips and shoulders. (The proximal muscles are those closest to the center of the body; distal muscles are farther away from the center — for example, in the hands and feet).
The shoulder girdle is the bony structure that surrounds the shoulder area, and the pelvic girdle is the bony structure surrounding the hips. Collectively, these are called the limb girdles, and it is the observed weakness and atrophy (wasting) of the muscles connected to the limb girdles that has given this group of disorders its name.
Together, the group of disorders that constitute LGMD is the fourth most common genetic cause of muscle weakness with an estimated worldwide prevalence between 0.8 and 6.9 in every 100,000 individuals. Approximately 5000 people are currently living with LGMD in the United States.
What are the symptoms of LGMD?
The unifying features of the LGMDs are the weakness and atrophy of the limb-girdle muscles. However, the age at which symptoms appear, and the speed and severity of disease progression, can vary.
Individuals may first notice a problem when they begin to walk with a “waddling” gait because of weakness of the hip and leg muscles. They may have trouble getting out of chairs, rising from a toilet seat, or climbing stairs. As this weakness progresses, the person may require the use of assistive mobility devices.
Weakness in the shoulder area may make reaching over the head, holding the arms outstretched, or carrying heavy objects difficult. It may become increasingly hard to keep the arms above the head for such activities as combing one’s hair or arranging things on a high shelf. Some people find it harder to type on a computer or other keyboard and may even have trouble feeding themselves.
Some of the LGMD subtypes also are characterized by additional symptoms. For example, the heart can be affected in some types of LGMD, with weakness of the heart muscle (cardiomyopathy) and/or abnormal transmission of signals that regulate the heartbeat (conduction abnormalities or arrhythmias).
Some disease subtypes also involve the muscles used for breathing, and for that reason, respiratory function, along with cardiac function, should be monitored regularly.
Other symptoms may be present in some of the different subtypes of LGMD, including but not limited to joint stiffness, muscle cramps, enlargement of calf muscles, and involvement of distal muscles of the body such as those controlling the hands and feet.
What causes LGMD?
Genes are the codes, or recipes, that cells use to manufacture the various proteins needed by the body. The genes associated with LGMD normally encode proteins that play vital roles in muscle function, regulation, and repair. When one of these genes contains a mutation (a flaw, such as missing or incorrect information), cells cannot produce the proteins needed for healthy muscles.
There are two major groups of LGMDs. Traditionally called LGMD1 and LGMD2, these two groups are classified by the respective inheritance patterns: autosomal dominant and autosomal recessive. If one copy of the abnormal gene is sufficient to cause the disease, it is said to be autosomal dominant; if two copies are needed, then the inheritance pattern is autosomal recessive. In some families, the inheritance pattern cannot be determined. For more details on the various inheritance patterns, see the NIH Genetics Home Reference.
Dozens of different genes, when mutated, have been shown to cause specific LGMD subtypes. In these cases, the proteins associated with these genes are nonfunctional or deficient, and muscles are unable to function normally. Gradually, the muscles become weak enough that people experience the symptoms of LGMD.
In addition to the known LGMD subtypes linked to specific genes, there are many cases of LGMD for which the causative gene is not yet known (and people with these cases are not identified as having a subtype-specific form of LGMD). Scientists are actively working to understand the causes of these unidentified subtypes of LGMD, because the more we understand about all the different causes of LGMD and the diverse ways that muscle can be compromised, the better chance we have of finding effective therapies to intervene in the pathological process.
What is the progression of LGMD?
At this time, progression in each type of LGMD cannot be predicted with certainty, although knowing the underlying genetic mutation can be helpful. Some forms of the disorder progress to loss of walking ability within a few years and cause serious disability, while others progress very slowly over many years and cause minimal disability.
LGMD can begin in childhood, adolescence, young adulthood, or even later. Both genders are affected equally.
When LGMD begins in childhood, some physicians say, the progression is usually faster and the disease more disabling. When the disorder begins in adolescence or adulthood, they say, it is generally not as severe and progresses more slowly. The course is usually one of slowly progressive, mostly symmetric weakness, with the exception of a few types with rapid progression or asymmetric weakness.
What is the status of research on LGMD?
MDA-supported scientists are pursuing several exciting strategies in muscular dystrophy research that have implications for LGMD. These strategies include gene therapy, exon skipping, stop codon read through, and myostatin blocking.
How are the LGMD subtypes classified?
The various subtypes of LGMD have traditionally been classified alphanumerically, with a 1 or 2 to designate dominant or recessive inheritance, and a letter added in order of discovery. An example is LGMD2A, in which 2 = recessive and A = first discovered. A new naming system has been proposed, however, leading to LGMD2A to also be referred to as LGMD R1-calpain3-related, with R = recessive, 1 = first discovered, and calpain3-related referring to the defective protein.
To learn more about neuromuscular diseases, including LGMD, see:
MDA’s Print-Ready Educational Materials
Additional reading
- Understanding Neuromuscular Disease Care. IQVIA Institute. Parsippany, NJ. (2018).
- Johnson NE, Statland JM. The Limb-Girdle Muscular Dystrophies. Continuum (Minneap Minn). 2022 Dec 1;28(6):1698-1714. doi: 10.1212/CON.0000000000001178. PMID: 36537976.
- Mah JK, Korngut L, Fiest KM, Dykeman J, Day LJ, Pringsheim T, Jette N. A Systematic Review and Meta-analysis on the Epidemiology of the Muscular Dystrophies. Can J Neurol Sci. 2016 Jan;43(1):163-77.)
- Bouchard C, Tremblay JP. Limb-Girdle Muscular Dystrophies Classification and Therapies. J Clin Med. 2023 Jul 19;12(14):4769. doi: 10.3390/jcm12144769. PMID: 37510884; PMCID: PMC10381329.
Last reviewed March 2025 by Chamindra Laverty, MD.

