Duchenne Muscular Dystrophy (DMD)
Research
Research in Duchenne muscular dystrophy (DMD) has advanced significantly over the past several decades, shifting from supportive care to targeted molecular therapies. Efforts now focus on restoring dystrophin production, improving muscle regeneration, reducing inflammation and fibrosis, and protecting the heart and diaphragm.
Many therapies are in late-stage clinical trials or have received U.S. Food and Drug Administration (FDA) approval under accelerated pathways. The goal is to combine complementary therapies for enhanced and durable benefit across all stages of disease.
Research
In DMD, muscle is missing a key structural protein called dystrophin, making it more susceptible to injury. Eventually the body cannot keep up with repair and regeneration, leading to muscle loss (wasting) and weakness. Broadly, scientists are working on the development of complementary therapies that can concurrently (1) protect the muscle from injury, (2) replace dystrophin, and (3) promote muscle repair and regrowth. Doctors hope that someday these potential therapies may be used in combination for maximum benefit.
Many examples of these potential therapies already have advanced into clinical trials where they are being evaluated for benefits in people with DMD. See MDA's Clinical Trial Finder for a list of clinical trials currently being conducted for DMD.
Therapeutic strategies under investigation to treat DMD include:
- Combating inflammation in muscle
- Inserting new dystrophin genes
- Controlling how cells read genetic instructions
- Driving muscle growth and regeneration
- Safeguarding muscle from damage
- Blocking muscle fibrosis
- Maximizing blood flow to muscle
- Protecting the dystrophindeficient heart
- Supporting appropriate maintenance and differentiation of muscle stem cells
Combating inflammation in muscle
During healthy muscle repair, inflammatory responses are activated and are known to aid in the cleanup and restoration of damaged muscle. In DMD, however, these inflammatory responses are pathologically chronically activated, becoming detrimental to the repair process. Scientists therefore are working to understand and interfere with inflammation in and around muscle fibers that may contribute to the DMD disease course.
Corticosteroids (such as prednisone, deflazacort, and vamoralone) are commonly used in DMD to help preserve muscle strength and function, to prevent scoliosis, and to prolong the time that people with DMD can walk. Corticosteroids work, at least in part, by non-specifically reducing inflammation within muscle, mitigating (but not reversing) the cycle of inflammation and regeneration. However, corticosteroids also cause unwanted side effects such as increased appetite, weight gain, loss of bone mass, psychological effects, and cataracts.
The FDA on Feb. 9, 2017, approved deflazacort (brand name Emflaza) to treat DMD for patients 5 years old and older. In June 2019, FDA approved Emflaza for the treatment of DMD in patients between 2 and 5 years old, allowing for earlier therapeutic intervention. This expansion was based on data from clinical studies demonstrating the efficacy and safety of Emflaza in younger patients.
MDA has invested heavily in researchers who developed the new anti-inflammatory therapy vamoralone, to have fewer and less severe side effects than prednisone and deflazacort. Vamorolone (Agamree) received FDA approval on October 26, 2023. Vamoralone is indicated for the treatment of DMD in patients aged 2 years and older. Ongoing studies continue to investigate the long-term efficacy of vamoralone versus prednisone and deflazacort.
Several experimental therapies are being studied to target inflammation in DMD, a key factor contributing to muscle degeneration. Monoclonal antibodies that block critical components of the immune system involved in inflammation, such as the IL-6 receptor and the interleukin-1 beta (IL-1β) cytokine, remain under investigation. Ongoing trials reflect the growing focus on immune-modulating therapies as a way to slow muscle degeneration and improve outcomes for individuals with DMD.
Inserting new dystrophin genes
Gene-targeted therapy refers to treatments that alter genetic activity. Technically, though exon skipping and gene silencing molecules affect RNA, rather than DNA, they are commonly still included under the umbrella term of “gene therapy” rather than the more cumbersome phrase of “transcriptome therapy”. Gene replacement therapy delivers a version of a healthy gene directly to a patient’s tissues, substituting the flawed gene for a less flawed gene. This therapeutic method is widely used to treat patients in multiple disease areas, with a growing knowledge base of the long-term effects.
In DMD, gene replacement therapy is a one-time therapy that delivers a miniaturized copy of the DMD gene, commonly referred to as “micro-dystrophin.” Scientists hope that by introducing a functional DMD gene, gene therapy may offer a more permanent benefit than other therapies. They are quick to caution, however, that gene therapy for DMD is unlikely to completely halt or reverse the disease. It is also noted that gene replacement occurs postnatally, or after birth, when significant damage has already occurred to muscle.
The most common strategy to accomplish gene therapy in DMD is to utilize the action of viruses. A virus works by inserting its own genetic material (i.e., microdystrophin) into a host (i.e., individual with DMD). Scientists have inserted a smaller version of the DMD gene into the virus, so the virus will deliver the modified DMD gene into muscle cells to manufacture a semi-functional dystrophin protein. To accomplish this without making the patient sick, they are utilizing viruses that do not cause illness in humans.
Research into the development of gene therapy for DMD is robust, but some challenges remain. The key difficulties to overcome include dealing with the large size of the DMD gene, delivering a sufficient quantity of the new genes to muscle (while avoiding other tissues), and mitigating an immune response to the virus and the newly generated microdystrophin proteins.
The large size of the DMD gene poses a challenge because gene therapy relies on engineered viruses such as adeno-associated virus (AAV), and there is a limit to the size of the load that these viruses can carry. The full-length DMD gene is significantly larger than the carrying capacity of AAVs. To address this, scientists have created smaller, but still functional, versions of the dystrophin gene to use in gene therapy. The miniaturized version of dystrophin, termed ‘microdystrophin’, is approximately one-third the size of the full dystrophin gene, but is capable of encoding a mostly functional dystrophin protein. The different microdystrophins used in clinical practice and in clinical trials were based on the DMD gene in BMD patients. The most common way to deliver microdystrophin gene therapy is using AAVs. Several companies now have gene therapy candidates for DMD in clinical trials, each with subtle differences between the engineered microdystrophin and chosen viral vectors.
In June 2023, the FDA granted accelerated approval for Elevidys (delandistrogene moxeparvovec-rokl), a microdystrophin gene therapy developed by Sarepta Therapeutics for the treatment of 4-5-year-old ambulatory DMD patients. In June 2024, the FDA further expanded this approval to ambulatory patients above 4 years old. Additionally, use of Elevidys in non-ambulatory patients received accelerated approval in 2024, with ongoing trials in progress to evaluate clinical benefit, safety, and durability of treatment.
To address delivery of genes specifically to muscles (while avoiding accidental activation in other tissues), researchers utilize muscle-specific promoters to “turn on” the transcription of the microdystrophin gene product, similar to a control switch for the new microdystrophin gene. Muscle-specific promoters selectively promote activation of the gene only when in muscle, but in other tissues the gene remains dormant so it cannot create unwanted side effects.
To receive gene therapy, individuals must not have antibodies to the particular AAV that is being utilized, and must not have specific gene mutations. The primary risks of gene replacement therapies result from the large inflammatory response to the virus and microdystrophin protein product, not uncommonly resulting in inflammation to the liver (transaminitis) and heart (myocarditis). Several new investigational gene therapies are being evaluated in ongoing clinical trials, each utilizing subtly different viral vectors, microdystrophin designs, and promoters to optimize delivery and function in muscle cells. Ultimately, the goal of gene replacement in DMD is to transform DMD into a BMD phenotype.
Controlling how cells read genetic instructions
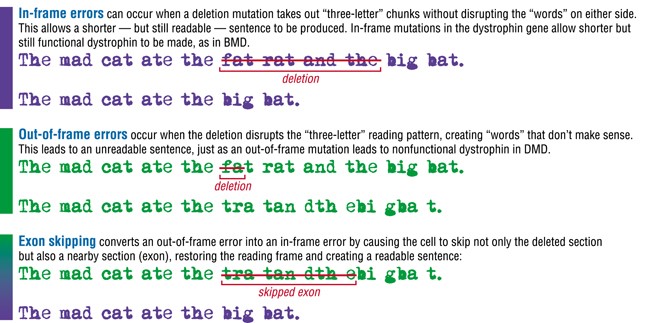
Exon skipping: Exon skipping is a strategy currently employed for DMD in which sections of genetic code (exons) are “skipped,” allowing the creation of partially functional dystrophin protein. Exon skipping is not expected to reverse muscle wasting that has occurred as a result of disease progression, but has the potential to modify the disease trajectory of DMD. To understand exon skipping, think of the genetic code for a protein as a sentence. Cells have to read the genetic “sentence” in units of three “letters” each.
For example:

On Sept. 19, 2016, the FDA granted accelerated approval to eteplirsen (brand name Exondys 51) as the first exon-skipping drug for DMD. Exondys 51 specifically targets a portion of the DMD gene called exon 51. It is estimated that 13% of boys harbor DMD mutations that are amenable to exon 51 skipping. The FDA has granted accelerated approvals to several additional exon-skipping therapies, including Vyondys 53 (golodirsen) for exon 53 in December 2019, Viltepso (viltolarsen) for exon 53 in August 2020, and Amondys 45 (casimersen) for exon 45 in February 2021. Each therapy targets different DMD exons to restore the reading frame and produce a truncated but functional dystrophin protein. Exon-skipping strategies can be beneficial, but currently only treat approximately 30% of patients because of the mutation-specific nature of these therapies. Additionally, current exon-skipping drugs require weekly infusions, impacting quality of life.
Next generation exon-skipping therapies are now being developed that target a broader range of exons to skip, have improved efficacy and penetration, and require decreased infusion frequency. Newer strategies are being designed with modified genetic sequences, chemistry, and backbone structures to improve delivery into skeletal and cardiac muscles. One approach involves the use of peptide- or antibody-based-delivery tags that enable the therapies (known as antibody oligonucleotide conjugates or AOCs) to get into specific cell types in the body. The goal is to enhance targeting of these therapies into skeletal and cardiac muscles so that they are more effective at boosting dystrophin levels in the tissues most affected in DMD. At least 10 other exon skipping drugs remain in development, targeting exons 44, 43, 55, 52, and 8. If approved, these therapies would together treat 60-80% of DMD patients.
Stop-codon read-through: Some mutations in the DMD gene create premature stop codons (also called nonsense mutations), which tell the cell’s inner machinery to stop making the dystrophin protein before it has been completely assembled. Certain drugs are designed to trick the cell’s machinery to ignore, or "read through," the inappropriately created premature stop codon in a gene, theoretically resulting in translation of functional protein. Between 5% and 10% percent of people with DMD have premature stop codon/nonsense mutations and may therefore someday benefit from read-through therapies.
An experimental stop codon read-through drug called ataluren (PTC124) was developed with funding from MDA by PTC Therapeutics, in conjunction with Genzyme Corp., to treat DMD or BMD due to a premature stop codon. Ataluren (brand name Translarna) was granted conditional marketing authorization in the European Union in August 2014. This made it the first therapy approved in the EU to treat certain patients with DMD caused by nonsense mutations. The conditional authorization has been renewed periodically based on ongoing data collection and real-world evidence. Translarna continues to have conditional approval in the European Union for nonsense mutation DMD, though it has not been approved by the FDA in the United States.
Researchers are also exploring therapeutic strategies that use specially designed molecules called transfer RNAs (tRNAs) to overcome premature stop codons. These tRNA-based therapies allow the cell to keep making the dystrophin protein even when there is a premature stop codon in the DMD gene. Some groups are investigating ways to deliver these tRNAs more effectively (e.g., lipid nanoparticles, exosomes) to increase the specificity and efficiency of tRNA therapies. At present, tRNA-based strategies are still in early stages of research and testing.
Driving muscle growth and regeneration
A prominent symptom of DMD is muscle loss, so researchers aim to develop therapies that promote regrowth of quality muscle to subsequently increase muscle strength.
One strategy involves inhibiting the actions of myostatin, a naturally occurring protein that limits muscle growth. In healthy muscle, myostatin performs an important role: it resists growth signals to maintain muscle at a reasonable size. In DMD, where muscle loss contributes to functional decline, the actions of myostatin exacerbate muscle loss. Thus, inhibiting myostatin’s function may allow the muscles of individuals with DMD to grow larger and stronger.
Myostatin inhibitors have received much attention from the neuromuscular disease research community as people and animals with genetic deficiencies of myostatin function appear to have large muscles and good strength without apparent ill effects.
Several companies have developed and tested myostatin inhibitors, but these have not resulted in significant functional improvement in clinical trials. These outcomes highlight the challenges of targeting myostatin in DMD treatment.
Another unique strategy to block the action of myostatin uses gene therapy to introduce follistatin, a naturally occurring inhibitor of myostatin. Mice with a DMD-like disease that received genes for the follistatin protein showed an overall increase in body mass and weight of individual muscles. Furthermore, monkeys that received follistatin gene transfer had stronger, larger muscles. Gene therapy to introduce follistatin to treat DMD patients has been studied in early-stage clinical trials.
Stem Cells: Stem cells are normally present in a variety of tissues, including muscle, where they are termed “myoblasts” and play a crucial role in repair and maintenance. Stem cells can be thought of as cells that are in the very early stages of development, before they have become specialized (differentiated) to perform specific roles in tissues. They may be precursors to a specific cell type (such as muscle or nerve cells) or they may still retain pluripotency — the ability to develop into any of a number of different cell types. In adults and children, stem cells reside in muscle tissue where they remain dormant until the tissue is damaged by injury or disease and it is required for them to synthesize more muscle. Following tissue damage, stem cells become activated and then replenish the damaged tissues. In DMD, it is known that the “reserve” of muscle stem cells is gradually depleted because of the perpetual cycles of injury and regeneration. Several stem cell strategies remain in focus for DMD. Most directly, the direct replacement or transplant of healthy muscle stem cells into patients with DMD may boost muscle growth. Alternatively, activating myoblasts with small molecules to create more muscle, rather than fibrotic and fatty tissues, remains an ongoing area of investigation.
One type of stem cell that holds a lot of promise for transplant is called an induced pluripotent stem cell (iPS cell). This type of cell is derived from adult cells in a process that was pioneered by Dr. Shinya Yamanaka’s lab in Japan. In 2012 he was awarded the Nobel Prize for this work.
A team of MDA-supported scientists led by Dr. Rita Perlingeiro have invented and continue to refine a method to efficiently generate immature skeletal muscle cells from iPS cells. Dr. Perlingeiro's laboratory, in conjunction with Myogenica, has been at the forefront of developing an induced pluripotent stem cell (iPSC)-derived muscle stem cell product (MyoPAXon) designed to regenerate skeletal muscle in DMD patients. The therapy involves reprogramming patient-derived cells into iPSCs, which are then differentiated into muscle progenitor cells capable of engrafting into muscle tissue and producing dystrophin. This approach aims to restore muscle function and halt disease progression, with ongoing clinical trial investigation.
In addition to stem cell transplantation, scientists are exploring the potential to use a more traditional drug approach to activate a patient’s own muscle stem cells. These muscle stem cells, called satellite cells because of their position next to muscle cells, naturally exist to perform muscle repair. Preliminary work by several labs has shown that satellite cells become activated following inhibition of enzymes called histone deacetylases (HDACs).
Building upon preclinical studies demonstrating that HDAC inhibition can induce muscle growth, reduce inflammation, and decrease fibrosis in DMD mouse models, Italfarmaco developed givinostat, an HDAC inhibitor. In March 2024, the FDA approved givinostat, marketed as Duvyzat, for the treatment of DMD in patients aged six years and older, regardless of their specific genetic mutation. Givinostat functions by targeting pathogenic processes to reduce inflammation and muscle degeneration.
These developments underscore the need to develop muscle regenerative strategies in addition to genetic correction strategies for a multi-pronged approach to treating DMD.
Safeguarding muscle from damage
DMD muscle is more susceptible to damage because it is missing dystrophin, a protein that sits at the muscle cell membrane and is critical for maintaining the muscle’s structural integrity. Thus, scientists have devised a number of potential therapies to make DMD muscle more resilient to injury.
One strategy is to compensate for the lack of dystrophin with a similar muscle protein, utrophin. Utrophin is a naturally occurring structural protein that closely resembles dystrophin and performs a very similar function in the muscle. A key difference is that utrophin is produced during muscle development or early-stage muscle repair. Production of utrophin is turned off during early development and replaced by production of dystrophin (except for in the area where the nerves and muscles meet, where utrophin continues to be present in adult tissue). Scientists believe that if utrophin production were turned back on, it may be able to compensate for the absence of dystrophin.
Several clinical trials have investigated utrophin modulators. While these specific compounds did not yield successful outcomes, research into utrophin modulation persists. Efforts are ongoing to identify and develop alternative molecules with improved efficacy and pharmacokinetic profiles to harness utrophin upregulation as a viable therapeutic approach for DMD.
Another novel approach to treating DMD and BMD is using Sevasemten (EDG-5506), a fast-myosin modulator developed by Edgewise Therapeutics. This therapy targets fast-twitch skeletal muscle fibers, which are preferentially susceptible to injury in dystrophinopathies. Sevasemten selectively inhibits fast skeletal muscle myosin, the motor protein responsible for muscle contraction, thereby reducing injury to muscle. Sevasemten’s ability to stabilize muscles and enhance long-term treatment outcomes continues to be studied in phase 2/3 clinical trials.
A third strategy to fortify DMD muscle is to introduce a different naturally occurring structural protein called laminin 111. The introduction of laminin 111 was shown to improve exercise capacity, increase muscle strength, and reduce muscle damage in a mouse model of DMD. This work was pioneered by MDA-funded scientist Dean Burkin.
Researchers also are exploring whether muscle integrity could be strengthened by the introduction of an enzyme called beta-1,4-N- acetylgalactosamine galactosyltransferase (GALGT2) using gene-targeted therapy. GALGT2 is involved in adding sugar molecules to a protein called alpha-dystroglycan, which is part of a cluster of proteins located at the muscle fiber membrane. This cluster is abnormal in DMD muscle. It has been shown that raising GALGT2 levels in mice can help to compensate for the loss of dystrophin and protect muscle from damage. Gene therapy to introduce GALGT2 for treatment of DMD patients is being studied in early-stage clinical trials.
The repeated bouts of damage that occur in DMD muscle have been shown to eventually induce death (necrosis) of the muscle cells. Scientists believe that therapies that block the signals that contribute to cell death may one day be used to slow muscle degeneration and, in turn, loss of function.
Scientists also have identified regulation of calcium in muscle as a potential strategy for therapeutic intervention. Because of the problems with the muscle cell membrane (sarcolemma) in DMD, calcium accumulates to pathologic levels in muscle cells, ultimately degrading muscle proteins and leading to cell death. There is evidence that calcium plays an important role in disease progression in DMD muscle, so several groups are investigating ways to appropriately taper accumulation of calcium in DMD muscle cells. One approach being explored is inhibiting a protein channel called TRPC6, which normally lets calcium into cells and may contribute to muscle damage in DMD. Another approach aims to reduce intracellular sodium and calcium overload in DMD muscle cells. While therapies targeting calcium regulation are promising, further clinical studies are required to determine their effectiveness in reducing muscle damage and improving function in DMD patients.
Blocking muscle fibrosis
As muscles degenerate in a person with DMD, the muscle fibers are replaced by fat and connective tissue in a process called fibrosis. Fibrosis is also called scarring, and the presence of fibrotic tissue in muscle impedes proper function and repair. Not unexpectedly, scientists have observed that the extent of fibrosis in DMD muscle correlates with diminished function. Thus, MDA-supported researchers are investigating whether muscle function might be protected by medications, termed anti-fibrotics, that reduce fibrosis. In addition, scientists hope that reducing fibrosis also may help increase the efficacy of other potential therapies.
Targeting connective tissue growth factor (CTGF) is a common mediator of fibrotic disease. Preclinical research has demonstrated a benefit of inhibiting CTGF in a mouse model of DMD. This work showed that CTGF reduces the ability of damaged muscle cells to repair themselves and promotes muscle fibrosis, and that inhibiting CTGF reduced muscle fibrosis and improved muscle function. Although an antibody-based therapy targeting CTGF was evaluated in clinical trials, no such therapy has yet demonstrated a successful outcome.
Maximizing blood flow to muscle
People with DMD experience inadequate blood flow to their muscles while exercising, which may contribute to fatigue and reduced performance. Thus, scientists hope that drugs that restore proper blood flow to muscles may benefit muscle strength and function.
Experiments have shown that, when dystrophin is missing from the muscle fiber membrane, it causes another protein known as neuronal nitric oxide synthase (nNOS) to be missing as well. This results in an inability of the blood vessels supplying muscles to adequately dilate during exercise, leading to fatigue. Phosphodiesterase inhibitors are a class of drugs that dilate blood vessels; examples include sildenafil (Viagra) and tadalafil (Cialis), both used to treat erectile dysfunction and pulmonary arterial hypertension. When nNOS-deficient mice were treated with a phosphodiesterase inhibitor, their exaggerated fatigue response to exercise was eliminated.
On the basis of these and other findings, researchers have started investigating the possibility that phosphodiesterase inhibitors can improve muscle function in people with DMD or BMD. Of note, some research has focused on the effects of phosphodiesterase inhibitors on heart function in DMD and BMD.
Protecting the dystrophin-deficient heart
DMD heart muscle, like skeletal muscle, is more susceptible to damage because it is missing dystrophin, an important structural component of the cell membrane. As a result, most affected people develop heart damage, also termed cardiomyopathy, weakening the heart’s ability to contract and pump blood to the rest of the body.
To address DMD-associated cardiomyopathy, researchers are aggressively pursuing several strategies to sustain or improve heart function beyond traditional heart failure medicines as previously discussed in the management section. They are testing already existing medications for their possible benefits in the DMD-affected heart and conducting research to find new approaches to specifically treat the dystrophin-deficient heart.
Because several cardiomyopathy drugs have been developed over the years to treat heart failure in older patients, doctors already have some tools at their disposal for treating the DMD heart. These therapies center on ways of reducing the burden on the pumping heart. To that end, doctors may prescribe angiotensin converting enzyme inhibitors (ACE inhibitors) and angiotensin receptor blockers (ARBs) that make blood vessels open wide and thereby reduce the resistance to the heart’s pumping action. Diuretics may be prescribed to remove extra water from the blood, so that there is less volume for the heart to pump. Beta-blockers may be prescribed to slow the heart rate, giving the DMD heart sufficient time to empty and refill with each beat so that it can pump blood more efficiently. Aldosterone antagonists (spironolactone or eplerenone) may be prescribed to protect the heart from worsening injury. Most recently, SGLT2-inhibitors (canagliflozin, dapagliflozin, and empagliflozin) have started to be used for their multiple benefits to protect the heart, kidneys, and combat metabolic syndrome.
Researchers are continuing to study existing drugs to determine the best regimen to preserve heart function in DMD.
Last reviewed May 2025 by Stephen Chrzanowski M.D., Ph.D.

