Myasthenia Gravis (MG)
Myasthenia Gravis (MG)
What is myasthenia gravis?
 Myasthenia gravis (MG) is an autoimmune disease — a disease that occurs when the immune system attacks the body’s own tissues. In MG, that attack interrupts the connection between nerve and muscle — the neuromuscular junction. Myasthenia gravis is characterized by
Myasthenia gravis (MG) is an autoimmune disease — a disease that occurs when the immune system attacks the body’s own tissues. In MG, that attack interrupts the connection between nerve and muscle — the neuromuscular junction. Myasthenia gravis is characterized by
autoantibodies against the acetylcholine receptor (AChR-Ab), or against a receptor-associated protein called muscle-specific tyrosine kinase (MuSK-Ab)
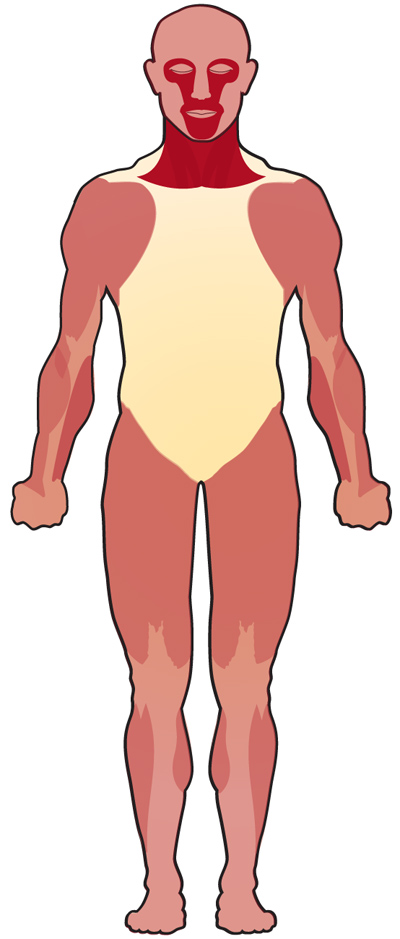
There are two clinical forms of myasthenia gravis: ocular and generalized. In ocular myasthenia gravis, muscle weakness often first appears in the muscles of the eyelids and other muscles that control movement of the eye (extraocular muscle). In generalized MG, the weakness involves the ocular muscles and a variable combination of the arm, legs, and respiratory muscles.
Myasthenia gravis is a relatively uncommon disease, with a prevalence of about 14 cases per 100,000 1,2 MG can occur at any age; the data presents a peak among females in their second decade of life and older males in their sixth to eighth decades.3 Autoimmune juvenile myasthenia gravis accounts for about 10% to 15% of the diagnosed cases in North America.4
The disease first appeared in medical reports in 1672, but did not earn its name, which literally means “grave muscular weakness,” until the 1880s.
What are the symptoms of MG?
MG causes weakness in muscles that control the eyes, face, neck, and limbs. Symptoms include partial paralysis of eye movements, double vision and droopy eyelids, as well as weakness and fatigue in neck and jaws with problems chewing, swallowing, and holding up the head. The hallmark of the disorder is a fluctuating degree and variable combination of weakness in ocular, bulbar, limb, and respiratory muscles. These symptoms may not always present and may shift from mild to severe repeatedly. The fluctuation of symptoms is an important feature that helps neurologists to distinguish MG from other disorders. Eventually, the diagnosis of MG can be established both by clinical and serologic testing (See Diagnosis).5
For more, see Signs and Symptoms.
What causes MG?
The cause of MG is unclear. Researchers suspect viruses or bacteria might trigger the autoimmune response; the thymus gland also seems to sometimes play a role in the disease. About 10% to 15% of those with MG have an underlying thymoma, a thymic tumor. Resection of the thymus, chemotherapy, and radiation therapy are likely to be recommended by the physician.
Autoimmune thyroid disease is seen in 3% to 8% of patients with MG. Screening for thyroid abnormalities should be part of the initial evaluation.
Although MG is not hereditary, genetic susceptibility appears to play a role in it and other autoimmune diseases. For more, see Causes/Inheritance.
What is the progression of MG?
MG is treatable with drugs that suppress the immune system or boost the signals between nerve and muscle. Surgeries and other procedures are also helpful in many cases. Most people with the disease are able to manage their symptoms and lead active lives, and a few experience remissions lasting many years. In about 10% to 15% of cases, MG begins in childhood (juvenile onset), which tends to progress slowly and has a high incidence of remission.
What is the status of research on MG?
MDA-supported scientists in countries around the world are working to reveal numerous facets of MG, from identifying possible causes and triggers to understanding the disease's molecular underpinnings to developing specific treatment strategies. For more, see Research.
For stories of families living with MG, see our MG stories on Strongly, the MDA blog.
Download our Myasthenia gravis (MG) Fact Sheet
References
- Understanding Neuromuscular Disease Care. IQVIA Institute. Parsippany, NJ. (2018).
- Carr, A. S., Cardwell, C. R., McCarron, P. O. & McConville, J. A systematic review of population based epidemiological studies in Myasthenia Gravis. BMC Neurol. (2010). doi:10.1186/1471-2377-10-46
- Boldingh, M. I. et al. Increased risk for clinical onset of myasthenia gravis during the postpartum period. Neurology (2016). doi:10.1212/WNL.0000000000003339
- Andrews, P. I. Autoimmune myasthenia gravis in childhood. Seminars in Neurology (2004). doi:10.1055/s-2004-829591
- Keesey, J. C. Clinical evaluation and management of myasthenia gravis. Muscle and Nerve (2004). doi:10.1002/mus.20030

