Grantee: Anne Connolly, M.D.
Funded: 9/1/2022 - 8/31/2025
Grant Type: Clinical Research Grant
Disease(s): Duchenne muscular dystrophy (DMD), Becker muscular dystrophy (BMD)

Duchenne muscular dystrophy (DMD) leads to weakness which, in infants and young boys manifests as slow motor development. Slow motor development means that boys with DMD walk and run later than other children. We recently showed that development could be improved by having the boys take liquid prednisolone at a dose of 10mg per kg per week in two divided doses of 5 mg per kg per day on two consecutive days. In that study of 24 infants and young boys (ages 3 months to 30 months), we showed this dose was safe. Only one boy stopped the prednisone because of side effects of irritability. All boys maintained normal linear growth using this intermittent dosing. The one important side effect was that about half of the boys gained more weight than expected for their age. Recently work in the mdx mouse (a good model of DMD) and older boys with DMD showed that smaller doses may work equally well. Here we plan to test a dose of 5mg/kg/week given on a single weekend dose. We will use a developmental scale called the Bayley-4 to assess the effects of this dose of prednisolone on motor development.
Grantee: Anne Connolly, M.D.
Grant type: Clinical Research Grant
Award total: $300,000.00
Institution: The Research Institute at Nationwide Children's Hospital
Country: Ohio, United States
Grantee: Paolo Grumati, Ph.D
Funded: 9/1/2022 - 8/31/2023
Disease(s): Congenital muscular dystrophies (CMD), Becker muscular dystrophy (BMD)
Muscular dystrophies are genetic disorders characterized by progressive muscle degeneration. In the severe forms, muscle deterioration predisposes patients to a wheelchair and cardiorespiratory failure, as is the case with Duchenne Muscular Dystrophy (DMD) and Ullrich Congenital Muscular Dystrophy (UCMD). DMD and UCMD are widespread worldwide and currently has no cure. These diseases are degenerative and existing treatments only address some of the symptoms, offering no real delay in disease progression. Muscle wasting in patients is characterized by an impairment of the autophagy process that is responsible for the removal of altered organelles inside the myofibers. Moreover, muscles present an increase of ER stress markers suggesting that ER homeostasis is compromised too. Despite its irreplaceable role in muscle physiology, when dysfunctional, the sarcoplasmic reticulum (SR) progressively loses its beneficial role in dystrophic muscles and becomes detrimental promoting a stressful environment and the consequent myofibers’ death. The mechanisms responsible for the fitness of the SR are still poorly understood, which limits any therapeutic efforts in this area. Therefore, investigating SR dynamics and its turnover, in DMD and UCMD muscle, is required to develop alternative therapeutic approaches. This research aims to uncover the biological mechanisms responsible for SR homeostasis. So doing, we hope to reveal targets for future pharmacological treatments.
Grantee: Paolo Grumati, Ph.D
Grant type: Idea Award
Award total: $50,000.00
Institution: Fondazione Telethon
Country: Italy
Grantee: Carrie Miceli, PhD
Funded: 11/1/2022 - 10/31/2024
Grant Type: MDA Request for Applications
Disease(s): Duchenne muscular dystrophy (DMD), Becker muscular dystrophy (BMD)

Micro-dystrophin GT aims to replace the missing dystrophin protein to normalize myofiber fragility and repair in DMD. However, because micro-dystrophin has never been previously expressed in DMD recipients, a risk remains for its recognition by host immunity as a foreign entity, triggering immune attack of cells expressing the transgene. We developed and implemented technology for simultaneous single nuclei RNA sequencing of multi-and mononucleated muscle resident cells to characterize cellularity and gene expression differences between healthy and DMD muscle, creating a snRNAseq reference set. Here we propose to perform snRNAseq on muscle biopsies from post micro-dystrophin GT to assess intra-muscular cell composition and gene expression changes, inclusive of immune and myo-lineage cells, induced by long-term micro-dystrophin expression (Aim 1). Given recent findings linking some micro-dystrophin T cell responses with accelerated muscle weakness and other toxicities, we focus on T cell response to micro-dystrophin. Muscle infiltrating T cells will be additionally characterized by single cell RNA sequencing, determination of paired TCR usage and antigen specificity (Aim 2). These studies promise to better identify "at risk patient DMD genotypes", "the nature of dystrophin immunoreactive epitopes", inform "design of in vitro assays predictive of transgene-triggered immune response" and "development of immunosuppression strategies to minimize transgene-triggered responses".
Grantee: Carrie Miceli, PhD
Grant type: MDA Request for Applications
Award total: $199,962
Institution: The Regents of the University of California, Los Angeles
Country: California, United States
Grantee: Jeffrey Chamberlain, PhD
Funded: 11/1/2022 - 10/31/2024
Grant Type: MDA Request for Applications
Disease(s): Duchenne muscular dystrophy (DMD), Becker muscular dystrophy (BMD)

Gene therapy for DMD is aimed at treating the cause of the disorder: a lack of dystrophin. Currently, the only known method for dystrophin delivery to muscles bodywide is by infusion of adeno-associated viral (AAV) vectors carrying miniaturized dystrophin genes. These AAV-microdystrophin (µDys) vectors have shown dramatic effects in animal models and are being tested in clinical trials. However, the observation of serious adverse events (SAEs) in 5 patients who were missing (deleted for) a part of the gene that is carried by µDys vectors has shown that parts of dystrophin can lead to a serious immune response in some patients. The immediate consequence of this has been that such patients (10-15% of all DMD boys) are being excluded from gene therapy trials. Our group has been studying dystrophin immunity for many years due to concerns that such a situation might emerge, and we have developed a computational method to predict immunogenic regions of dystrophin and to redesign vectors to remove problematic parts of the protein. To date we have successfully redesigned several portions of micro/mini-dystrophin and shown that they can be functional, stable and non-immunogenic in animal models. Here we propose to extend these studies to the problematic region recently identified in the clinic. Our goal is to develop modified dystrophin clones that could be used in clinical trials and thus allow broad enrollment of patients regardless of their underlying genetic mutation.
https://doi.org/10.55762/pc.gr.159120
Grantee: Jeffrey Chamberlain, PhD
Grant type: MDA Request for Applications
Award total: $200,000
Institution: University of Washington
Country: Washington, United States
Grantee: Tejvir Khurana, MD, Ph.D.
Funded: 9/1/2022 - 8/31/2025
Grant Type: Research Grant
Disease(s): Duchenne muscular dystrophy (DMD), Becker muscular dystrophy (BMD)

Duchenne's Muscular Dystrophy (DMD) is an incurable, genetic disease caused by mutations in the DMD gene leading to an absence of the dystrophin protein. Increased expression of a closely related gene called utrophin can rescue the disease, and increasing utrophin expression is considered a promising therapeutic strategy for DMD. Here we will harness post transcriptional mechanisms that regulate utrophin expression by gene editing to increase utrophin expression as a strategy for DMD gene therapy.
https://doi.org/10.55762/pc.gr.157006
Grantee: Tejvir Khurana, MD, Ph.D.
Grant type: Research Grant
Award total: $300,000
Institution: The Trustees of the University of Pennsylvania
Country: Pennsylvania, United States
Grantee: Forum Kamdar, PhD
Funded: 9/1/2022 - 8/31/2025
Grant Type: Clinical Research Network Grant
Disease(s): Duchenne muscular dystrophy (DMD), Becker muscular dystrophy (BMD)

Muscular dystrophies affect not only the muscle but the heart and can result in severe heart failure. Heart transplant and heart pumps, which are called ventricular assist devices, are used in patients with advanced heart failure and improve their quality of life and survival. There have been concerns about involvement of multiple organs and the ability to do physical rehabilitation after heart transplant or heart pumps for patients with muscular dystrophies, which has limited the use of these life saving therapies in patients with muscular dystrophies. We currently have data on heart transplant in muscular dystrophies from databases showing that it is safe, however the database does not collect information that is important for consideration of patients with muscular dystrophies like lung function or use of a wheelchair. Also, there are only reports of heart pump use in patients with muscular dystrophies and no larger databases with this information. Here we combine data from large muscular dystrophy and advanced heart faillure centers to look at the outcome and survival of patients who have muscular dystrophies who undergo heart transplant or heart pump treatment. Multiple centers are needed to have enough patients to understand the outcome of heart failure treatment in muscular dystrophy patients. This work has the potential to have a direct benefit to patients with muscular dystrophy by addressing a gap in their current heart care.
https://doi.org/10.55762/pc.gr.157024
Grantee: Forum Kamdar, PhD
Grant type: Clinical Research Network Grant
Award total: $198,000
Institution: Regents of the University of Minnesota - Twin Cities
Country: Minnesota, United States
Grantee: Alexia Kagiava, PhD
Funded: 9/1/2022 - 8/31/2023
Disease(s): Charcot-Marie-Tooth disease (CMT)

One of the major challenges in developing therapeutics for inherited neuropathies is to achieve adequate access of drugs and gene therapy agents into the peripheral nerves throughout the body through a clinically applicable delivery route. The blood-nerve barrier (BNB) limits this distribution and the effectiveness of potential therapies. In order to overcome this, we propose to test an innovative method by transiently disrupting the BNB using a Focused-Ultrasound System (FUS). We will then test the efficacy of this method to facilitate penetration of viral vectors for gene therapy into peripheral nerves. As model disease, X-linked Charcot-Marie Tooth Disease (CMT1X) is a common inherited demyelinating neuropathy, characterized by progressive muscle atrophy, weakness and sensory loss in the limbs. CMT1X is caused by mutations affecting connexin32 (Cx32), a protein that is expressed specifically by myelinating cells in the nerves, the Schwann cells, and plays important role in nerve function and integrity. Using a previously developed gene therapy vector for treating CMT1X, we will examine the benefit of transient BNB disruption using FUS in order to maximize the gene delivery to Schwann cells and the therapeutic efficacy. Successful application of this technique can also benefit several other therapy approaches for inherited neuropathies as well.
https://doi.org/10.55762/pc.gr.157047
Grantee: Alexia Kagiava, PhD
Grant type: Idea Award
Award total: $50,000
Institution: The Cyprus Foundation for Muscular Dystrophy Research
Country: Cyprus
Grantee: Bernard Jasmin, PhD
Funded: 9/1/2022 - 8/31/2025
Grant Type: Research Grant
Disease(s): Myotonic dystrophy (DM)

Myotonic Dystrophy type 1 (DM1) is caused by a mutation affecting the normal function of the cell, causing the many symptoms characteristic of this disease. Our research led us to investigate AMPK signaling in DM1 muscle cells. We recently found that AMPK signaling is altered in DM1 muscle cells, and that the activation of AMPK with drugs and exercise is beneficial for the pathology. Here, we will build upon these initial findings and investigate the role of AMPK signaling in DM1. The characterization of this pathway in DM1 appears crucial and timely as this study will pave the way to a better understanding of the DM1 pathology while leading to the development of novel therapeutic strategies for DM1.
https://doi.org/10.55762/pc.gr.157012
Grantee: Bernard Jasmin, PhD
Grant type: Research Grant
Award total: $300,000
Institution: University of Ottawa
Country: Ontario, Canada
Grantee: Michio Inoue, Ph.D.
Funded: 9/1/2022 - 8/31/2025
Grant Type: Development Grant
Disease(s): Limb-girdle muscular dystrophies (LGMD)

Proteins are originally string-like polypeptide chains that are folded to form functional proteins. Chaperones help in the folding process or correct the folding of misfolded proteins. Therefore, when chaperones abnormality, the number of misfolded, non-functional proteins increases and eventually accumulates in the body. Many such chaperone diseases, called "chaperonopathies," are involved in neuromuscular diseases. Understanding the function of chaperones will lead to the development of treatments for chaperonopathies. Our group has shown that mutations in two genes, DNAJB6 and DNAJB4, cause muscle diseases. However, it is still unknown what "client" proteins the chaperones work on, how they correct the misfolding, and why only specific muscles are more severely impaired. I am trying to uncover the client proteins by manipulating cells to prevent a particular gene from working. In addition, since my preliminary experimental data suggest that the DNAJ proteins may interact with each other and work to correct folding, we will analyze this using cells and animal models in which the two DNA proteins are rendered inactive. In addition, we will explore why only specific muscles are strongly damaged using animal models and imaging techniques. If these things are clarified, it will lead to significant progress in developing therapies.
https://doi.org/10.55762/pc.gr.157003
Grantee: Michio Inoue, Ph.D.
Grant type: Development Grant
Award total: $209,510
Institution: Washington University in St.Louis
Country: Missouri, United States
Grantee: Shushu Huang, M.D.
Funded: 9/1/2022 - 8/31/2025
Grant Type: Development Grant
Disease(s): Limb-girdle muscular dystrophies (LGMD)

Muscular dystrophy is a group of diseases that cause progressive weakness and loss of muscle mass. Sarcoglycanopathies (SGPs) are a common but severe form of it, which affect hip and shoulder muscles. SGPs is an inherited disease with two mutations (variants) concurrently present in each of the chromosomes. Variants in four sarcoglycan (SG) genes can cause SGPs, named SGCA, SGCB, SGCG and SGCD. Currently, it is difficult to interpret a variant as pathogenic. Muscle biopsy or DNA sequencing is necessary for the patients to be diagnosed. Typically, variants predicted to produce no protein are easier to be interpreted as pathogenic, while missense, the most common type of variant in genes, are harder to interpret, leaving many suspected SGP patients without a definitive genetic diagnosis. The molecular feature of SGPs is the absence or reduced SG protein expression on the muscle cell membrane. We will use this feature to develop a high throughput functional assay and evaluate the pathogenicity of different variants. We will create a DNA library with all possible single nucleotide variants for an SG gene, then introduce them into cells. By flow cytometry, a technique used to detect the SG proteins on the cell surface, we will be able to predict the pathogenicity for each of the variants, especially difficult to interpret missense variants. This method will create a ‘look-up’ table to aid in the clinical interpretation of variants in patients with SGPs.
https://doi.org/10.55762/pc.gr.157030
Grantee: Shushu Huang, M.D.
Grant type: Development Grant
Award total: $210,000
Institution: Yale University
Country: Connecticut, United States
Grantee: Lindsey Hayes, M.D., Ph.D.
Funded: 9/1/2022 - 8/31/2025
Grant Type: Research Grant
Disease(s): ALS (amyotrophic lateral sclerosis)
Amyotrophic lateral sclerosis (ALS) is a fatal degenerative disease of motor neurons for which there is no curative therapies. Despite significant genetic and phenotypic variability, postmortem evaluation in 97% of ALS patients shows disruption of the essential RNA binding protein, TDP-43. TDP-43 critically regulates RNA processing within the nucleus of the cell, and its cytoplasmic mislocalization and aggregation in disease causes widespread RNA splicing defects and aggregate-mediated disruption of cellular homeostasis. TDP-43 is therefore an important therapeutic target, although the upstream causes that initiate the TDP-43 pathogenic cascade in ALS remain unknown. A major goal of our laboratory is to investigate the molecular regulation of TDP-43 trafficking in healthy cells and its disruption in disease. Our recent studies show a major role for TDP-43's normal, nuclear RNA binding partners in regulating TDP-43 localization. Surprisingly, we have also observed that a prolonged disruption of the cellular gradient of TDP-43 RNA targets can initiate aberrant TDP-43 cytoplasmic aggregation. Here, we will perform a detailed biochemical and molecular characterization of RNA-induced TDP-43 cytoplasmic aggregation in cell lines and human neurons, to advance our understanding of the beneficial versus deleterious interactions of TDP-43 with RNA.
https://doi.org/10.55762/pc.gr.157034
Grantee: Lindsey Hayes, M.D., Ph.D.
Grant type: Research Grant
Award total: $300,000
Institution: Johns Hopkins University School of Medicine
Country: Maryland, United States
Grantee: Amy Hanna, Ph.D.
Funded: 12/1/2022 - 11/30/2025
Grant Type: Research Grant
Disease(s): Myotubular myopathy

Muscle cells are constantly making new proteins that are needed to perform important skeletal muscle functions, like contraction and relaxation. Newly made proteins are carefully folded to ensure they function properly and can be transported to where they are needed in the cell. Normally when a protein misfolds it is removed before it can affect cellular health but in some muscle diseases these misfolded proteins remain in the cell. How these misfolded proteins affect the ability of muscle to function is poorly understood. Our work suggests that in some diseases the "garbage disposal" systems of muscle cells become overworked, allowing these misfolded proteins to buildup and cause cellular stress. This proposal will examine the factors that regulate protein folding and determine how the accumulation of misfolded proteins affects muscle contraction and relaxation. Our work will also determine whether these stress pathways are a viable target for alleviating muscle dysfunction in congenital myopathy.
https://doi.org/10.55762/pc.gr.157041
Grantee: Amy Hanna, Ph.D.
Grant type: Research Grant
Award total: $297,000
Institution: University of Queensland (UQ)
Country: Texas, United States
Grantee: Jonathan Glass, PhD
Funded: 1/1/2022 - 12/31/2022
Grant Type: Restricted Research Grant
Disease(s): ALS (amyotrophic lateral sclerosis)
There is an enormous need for a better understanding of the clinical, demographic, and genetic features that underlie the phenotypic variability of ALS. Indeed, it may be more accurate to define ALS as a “syndrome” defined by the commonality of clinical features and progression. The syndrome of ALS may encompass a number disease mechanisms that will require different approaches for therapeutic intervention, and one could hypothesize that our failures in clinical trials for ALS are due to the inclusion of multiple disease types, some of which are not responsive to the experimental drug under investigation. Thus, we need to better understand whether multiple mechanisms of ALS truly exist, and to do that we need to better define the disease by documenting phenotypes along with genetic, serologic, and physiological features of disease. This improved categorization of disease will result in the definition of specific disease features that will allow for clinical trials targeting specific disease mechanisms. The CRiALS project, supported by MDA funding, has generated a world-class clinical database and biobank for use locally, nationally, and internationally for discovery research focused on better defining the mechanisms of ALS, which will lead to drug targets and directed therapeutics.
https://doi.org/10.55762/pc.gr.154583
Grantee: Jonathan Glass, PhD
Grant type: Restricted Research Grant
Award total: $16,255
Institution: Emory University
Country: Georgia, United States
Grantee: Hibiki Fujita, Ph.D.
Funded: 9/1/2022 - 8/31/2025
Grant Type: Research Grant
Disease(s): Mitochondrial myopathies, Encephalomyopathies
Mutations in a mitochondrial protein, coiled helix coiled helix domain containing protein 10 (CHCHD10) cause neuromuscular diseases including mitochondrial myopathy and amyotrophic lateral sclerosis. Mitochondrial abnormalities cause metabolic imbalance that contribute to these disorders. In this application, we propose to treat a mouse model of mutant CHCHD10 disorder that show mitochondrial myopathy, motor neuron degeneration, and cardiomyopathy. Disease altering strategies are needed for CHCHD10 disorders, since there are none to date. We propose to test two distinct strategies, one specifically targeting CHCHD10 with a genetic approach to reduce CHCHD10 levels, and the other to modulate metabolic imbalance observed in the mutant mice with nutritional approaches. We will investigate the effect of these strategies in the disease course of the mutant mouse. Importantly, metabolic therapy approaches tested in this application could be extended to a larger group of neuromuscular disorders involving similar metabolic dysregulation.
https://doi.org/10.55762/pc.gr.157007
Grantee: Hibiki Fujita, Ph.D.
Grant type: Research Grant
Award total: $300,000
Institution: Weill Cornell Medicine
Country: New York, United States
Grantee: Asuka Eguchi, Ph.D.
Funded: 9/1/2022 - 8/31/2025
Grant Type: Development Grant
Disease(s): Duchenne muscular dystrophy (DMD), Becker muscular dystrophy (BMD)
Currently, there are three clinical trials testing microdystrophin in Duchenne muscular dystrophy (DMD) patients. Microdystrophins have shown promise in improving skeletal muscle function; however, little is known about efficacy in the heart as animal models used in preclinical testing do not manifest dilated cardiomyopathy. This is a critical gap in our knowledge, as dilated cardiomyopathy is the leading cause of death in DMD patients. My project capitalizes on cardiomyocytes differentiated from human induced pluripotent stem cells harboring dystrophin mutations. I will compare how well microdystrophin variants rescue functional deficits exhibited by dystrophin-deficient cardiomyocytes against minidystrophin, comprised of more domains of dystrophin. The outcome of this study will yield design principles for transgenes that can improve the functional deficits of DMD cardiomyocytes. This study will evaluate the efficacy of existing microdystrophin variants in the context of cardiomyocyte function and will establish a platform for assessing functional rescue in human cells, accelerating the development of therapies to delay the onset of heart failure.
https://doi.org/10.55762/pc.gr.157032
Grantee: Asuka Eguchi, Ph.D.
Grant type: Development Grant
Award total: $210,000
Institution: The Board of Trustees of the Leland Stanford Junior University
Country: California, United States
Grantee: James Dowling, M.D., Ph.D.
Funded: 9/1/2022 - 8/31/2023
Disease(s): Central core disease

Childhood genetic muscle diseases affect at least 250, 000 North Americans and significant quality of life and life expectancy. Despite their prevalence and impact, few therapies have been developed. Many NMDs are caused by genetic mutations that result in the loss of a critical protein. An attractive therapeutic strategy is to replace the missing or mutated gene through gene replacement therapy. This approach has been extremely successful for a small number of conditions, such as spinal muscular atrophy, where gene therapy dramatically increases survival. Currently, viral vectors such as adeno associated viruses (AAVs) are the main gene therapy delivery system. AAVs can only carry genes of limited size. However, nearly half of all human genes exceed this size restriction, and It therefore is not feasible to use AAVs for gene replacement therapy for a large proportion of genetic muscle diseases. This proposal will directly address and seek to overcome this critical therapeutic barrier. We hypothesize that lipid nanoparticles can deliver large genes in a safe and effective manner. We will test this hypothesis for a disease called RYR1 related myopathy, a severe genetic childhood muscle diseases. We will use lipid nanoparticles to deliver RYR1, one of the largest genes in the genome, to rescue a mouse model of the human disease. Our study’s success will open the door not only for gene therapy for RYR1, but for the whole group of disorders caused by large gene mutations.
https://doi.org/10.55762/pc.gr.157051
Grantee: James Dowling, M.D., Ph.D.
Grant type: Idea Award
Award total: $50,000
Institution: The Hospital for Sick Children
Country: Ontario, Canada
Grantee: Robert Dirksen, Ph.D.
Funded: 9/1/2022 - 8/31/2025
Grant Type: Research Grant
Disease(s): Congenital muscular dystrophies (CMD)
Tubular aggregate myopathy (OMIM #160,565 and #615,883) is an inherited skeletal muscle disease characterized by weakness, cramps, myalgia, and fatigue that primarily affects proximal muscles of the lower limbs. The aberrant presence in skeletal muscle of tubular aggregates, regular arrays of highly-ordered and densely packed tubules, represents the key histopathological hallmark of this disease. There is currently no cure or effective treatment for this debilitating muscle disease. This project will use a newly generated mouse model of tubular aggregate myopathy with characteristics that mimic the human disease (including age-dependent muscle weakness, increased fatigue, and tubular aggregates in skeletal muscle) to provide needed insight into the underlying pathophysiological mechanisms and to assess therapeutic potential of early intervention with an Orai1 inhibitor treatment and endurance exercise in mitigating disease progression.
https://doi.org/10.55762/pc.gr.157013
Grantee: Robert Dirksen, Ph.D.
Grant type: Research Grant
Award total: $300,000
Institution: University of Rochester
Country: New York, United States
Grantee: Sabine De La Porte, HDR
Funded: 9/1/2022 - 8/31/2023
Disease(s): Duchenne muscular dystrophy (DMD), Becker muscular dystrophy (BMD)

Duchenne muscular dystrophy, is a muscular degeneration characterized by the absence of a cytsoskeletal protein, dystrophin, leading to death around the age of 35 from cardio-respiratory failure. Without curative treatment, corticosteroid therapy is the only treatment currently used. Serious side effects are described as depression or muscle weakness. Our preliminary results on the oxytocin (OT) levels of patients before and after corticosteroid therapy) strongly support the hypothesis that the addition of OT could have beneficial effects on cardiac function, muscle regeneration and social behaviors in patients. Using the Mdx mouse model, we will assess the combination of OT and corticosteroid therapy on these parameters. As oxytocin is FDA approved, the feasibility of rapid clinical application is strong.
https://doi.org/10.55762/pc.gr.157050
Grantee: Sabine De La Porte, HDR
Grant type: Idea Award
Award total: $50,000
Institution: Institut National de la Santé et de la Recherche Scientifique
Country: France
Grantee: Sandrine Da Cruz, Ph.D.
Funded: 9/1/2022 - 8/31/2025
Grant Type: Research Grant
Disease(s): ALS (amyotrophic lateral sclerosis)

Despite identification of ALS-associated RNA binding proteins (RBPs) including TDP-43 and FUS (which also cause the second most frequent dementia, frontotemporal dementia or FTD), the disease mechanism(s) are unknown. The effort proposed here seeks to uncover this mechanism to support therapy development in familial ALS forms and beyond. Key questions to be tackled will be to understand the emerging critical functions of TDP-43 and FUS within motor neuron projections called axons and at their synapses, where the mutant forms are known to accumulate. We will thus investigate how mutations cause axonal degeneration and loss of their neuromuscular junctions (NMJs), which are the earliest hallmarks of ALS pathogenesis. In particular we will identify the FUS/TDP-43 mRNA targets along axons and NMJs and unravel the mechanisms underlying their local protein synthesis in health and ALS pathogenesis.
https://doi.org/10.55762/pc.gr.157008
Grantee: Sandrine Da Cruz, Ph.D.
Grant type: Research Grant
Award total: $300,000
Institution: VIBvzw
Country: Belgium
Grantee: Peter Currie, PhD
Funded: 9/1/2022 - 8/31/2025
Grant Type: Research Grant
Disease(s): Limb-girdle muscular dystrophies (LGMD)

Although a significant number of new genes and new mutations in known genes are being identified as the cause of congenital muscle diseases why and how these mutations cause disease is often less than clear. Specifically, the relationship between the congenital muscle disease symptoms and the genetic lesion is often complex. Some muscle diseases with the same clinical phenotype result from mutations in several different genes but, by contrast, mutations in the same gene can lead to different congenital muscle diseases with a different clinical outcomes. The disparity found in disease presentations is perhaps no more apparent than when considering the disease spectrum evident in patients with FKRP deficiency, which can present as a mild muscular dystrophy diagnosed late in life, through to a severe pathology of the newborn affecting sight, mental capacity and ambulation. We have therefore generated zebrafish models of this muscular dystrophy to fill this knowledge gap. Combining studies in zebrafish genetics, patient cell lines and biochemical approaches we surprisingly revealed that FKRP acts on a second novel muscle pathway, directing alterations on fibronectin an important muscle attachment protein. This study aims to understand the clinical significance of this finding and to determine if this mechanism can explain the different types of disease that mutations in FKRP cause. In addition we wish to explore the possible therapy options our new findings have provided.
https://doi.org/10.55762/pc.gr.157035
Grantee: Peter Currie, PhD
Grant type: Research Grant
Award total: $295,614
Institution: Monash University
Country: Australia
Grantee: Greg Cooper, Ph.D.
Funded: 9/1/2022 - 8/31/2025
Grant Type: Research Grant
Disease(s): Limb-girdle muscular dystrophies (LGMD)

Neuromuscular disorders (NMDs) comprise a heterogenous group of conditions associated with impaired nerve and muscle function that affect 1-10/100,000 individuals worldwide, the vast majority of which result from one or more genetic factors. Despite successes from single gene, gene panel, and exome or genome sequencing tests, there remains a large portion of patients suspected to have genetic NMDs but for whom no precise diagnosis can be made using current clinical or laboratory information; such patients often undergo a “diagnostic odyssey” in which many tests are conducted over many years without success. We hypothesize that many genetic variants that cause NMDs are missed by standard DNA testing methods. We will apply an exciting “long-read” genome sequencing technology called Circular Consensus Sequencing (CCS, also called “HiFi”) recently developed by PacBiosciences to a group of undiagnosed children suspected to have a congenital NMD. Preliminary data indicate that CCS/HiFi sequencing is far more accurate than standard sequencing, especially for complex genetic variants, and has great potential to detect pathogenic, diagnostic genetic variants that were previously overlooked. We aim to refine data and process quality and establish methods suitable for routine research and clinical use. Our study has potential to improve diagnostic yield and provide better information, and ultimately improve outcomes, for patients and families affected by NMDs.
Grantee: Greg Cooper, Ph.D.
Grant type: Research Grant
Award total: $294,803
Institution: HudsonAlpha Institute for Biotechnology
Country: Alabama, United States
Grantee: Chang Geon Chung, Ph.D.
Funded: 9/1/2022 - 8/31/2025
Grant Type: Development Grant
Disease(s): ALS (amyotrophic lateral sclerosis)

Amyotrophic lateral sclerosis (ALS) is a neurodegenerative disease that primarily affects motor neurons, leading to paralysis and death within 2-5 years for most patients. There is a growing consensus that disruption of the nuclear pore complex (NPC) which shuttles proteins and RNAs in and out of the nucleus, contributes to the disease, but both the cause and consequences of this impairment remain unclear. A key finding in motor neurons in ALS is that they have protein aggregation and upregulation of endoplasmic reticulum (ER) stress pathways. While the ER stress pathway may initially protect motor neurons against accumulating toxic protein aggregates, chronic ER stress is believed to contribute to toxicity and cell death in ALS. Indeed, the Amylyx drug AMX0035 being reviewed by the FDA for treatment of ALS, is believed to protect neurons by inhibiting ER stress. ER stress induces activation of the “unfolded protein response” (UPR), which relies on the communication between the nucleus and cytoplasm (NCT). Our proposal aims to study how NCT impairment—a state of incommunicado between the nucleus and cytoplasm—affects ER stress and UPR in ALS models. Furthermore, ER is an important organelle that helps assemble the NPC, and we will also examine how ER stress affects NCT. Establishing how NCT and ER stress interact in ALS have the potential to identify new therapeutic target for ALS.
https://doi.org/10.55762/pc.gr.157027
Grantee: Chang Geon Chung, Ph.D.
Grant type: Development Grant
Award total: $210,000
Institution: Johns Hopkins University School of Medicine
Country: Maryland, United States
Grantee: Jeffrey Chamberlain, PhD
Funded: 7/1/2022 - 6/30/2022
Grant Type: Restricted Research Grant
Disease(s): Duchenne muscular dystrophy (DMD), Becker muscular dystrophy (BMD)

Gene therapy for Duchenne muscular dystrophy is an extremely promising approach to therapy as it directly addresses the cause of the disorder- a lack of functional dystrophin protein. Our group has spent more than 30 year studying the structure and function of dystrophin and developing approaches for gene therapy. This work includes development of numerous micro-dystrophin clones, several of which are being tested in clinical trials. We also showed that AAV vectors could be used for systemic delivery of new genes to muscles, bodywide. However, while current AAV-microdystrophin vectors are showing significant benefit in the clinic, several limitations have been identified. Among these are a lack of full function from micro-dystrophins, lower levels of dystrophin production than are ideal, and some vector dose limitations due to adverse events. Our proposal explores a new way to make larger mini-dystrophins and even full-sized dystrophin by co-delivery of current and novel AAV vectors. Here we explore the potential of this system to improve upon approach for gene therapy of DMD and other neuromuscular disorders.
https://doi.org/10.55762/pc.gr.158724
Grantee: Jeffrey Chamberlain, PhD
Grant type: Restricted Research Grant
Award total: $233,243
Institution: University of Washington
Country: Washington, United States
Grantee: Serena Carra, Ph.D.
Funded: 9/1/2022 - 8/31/2025
Grant Type: Research Grant
Disease(s): Charcot-Marie-Tooth disease (CMT)

Motor neuropathies (dHMNs) and ALS share common underlying mechanisms, including degeneration of peripheral nerves. Dysfunction at the junction between nerve and muscle, the neuromuscular junction (NMJ), is an early event contributing to motor neuron (MN) loss in dHMNs and ALS, with active denervation/reinnervation occurring during the disease. Importantly, the regeneration of nerves and muscles occurs also during adulthood to enable the repair of NMJs and damaged muscles; however, the regenerative abilities decline with aging, when these diseases develop. It is fundamental to better understand how dysfunctions of the neuromuscular system lead to dHMNs and ALS. This project aims to unravel players and mechanisms responsible for MN and NMJ vulnerability in dHMNs and ALS. We focus on the gene HSPB3, which is a promising candidate because: 1) rare HSPB3 variants have been found in dHMNs and ALS patients; 2) we have shown that HSPB3 is a specialized chaperone engaged in muscle and MN differentiation; 3) we found that HSPB3 induction is impaired in MNs carrying a mutation linked to ALS. We hypothesize that deregulation of the pro-differentiation functions of HSPB3 may contribute to NMJ deterioration with aging and in disease. Using human MNs and muscle cells and neuromuscular organoids derived from iPS cells we will study how HSPB3 dysfunction leads to degeneration and assess if its targeting increases the regenerative capacity of the neuromuscular system.
https://doi.org/10.55762/pc.gr.157046
Grantee: Serena Carra, Ph.D.
Grant type: Research Grant
Award total: $299,910
Institution: University of Modena and Reggio Emilia (Università degli Studi di Modena e Reggio Emilia)
Country: Italy
Grantee: Luca Caputo, PhD
Funded: 9/1/2022 - 8/31/2025
Grant Type: Development Grant
Disease(s): Duchenne muscular dystrophy (DMD), Becker muscular dystrophy (BMD)
Duchenne muscular dystrophy (DMD) is a devastating disease affecting the musculature of young kids and boys caused by mutations in the dystrophin gene, this in turn cause the absence of dystrophin protein, a protein that is essential to keep the muscle intact. DMD is characterized by a progressive replacement of musculature by fibrotic and fat tissue, this replacement causes dramatic loss of contractile function of the muscle. This disease causes kids to be wheelchair bound in their early teen years and death within the second/third decade of their life. Current therapeutic approaches have improved life expectancy; however, there is not yet a definitive cure of the disease. In this project I propose a novel approach to understand if reintroduction of dystrophin in muscles is able to repair all the damages that muscles have acquired. Understanding this, will allow to identify future therapeutic targets to cure DMD.
https://doi.org/10.55762/pc.gr.157010
Grantee: Luca Caputo, PhD
Grant type: Development Grant
Award total: $210,000
Institution: Sanford Burnham Prebys Medical Discovery Institute
Country: California, United States
Grantee: Alessandra Bolino, Ph.D.
Funded: 10/15/2022 - 10/14/2025
Grant Type: Research Grant
Disease(s): Charcot-Marie-Tooth disease (CMT)

(Co-funded with CMT Research Foundation)
Charcot-Marie-Tooth (CMT) neuropathies are generally characterized by progressive muscular atrophy and weakness, with an age at onset usually comprised between the first and the second decade of life. Among CMT neuropathies, CMT4B1 is a very severe demyelinating neuropathy with childhood onset, characterized by myelin outfoldings, redundant loops of myelin in the nerve that degenerate causing axonal problems. This form of aberrant myelin is also a pathological feature of other forms of demyelinating CMT, such as CMT4B2, B3, CMT4C and CMT4H. Our laboratory demonstrated that loss of MTMR2 (Myotubularin-related 2) phosphatase is the cause of the disease. MTMR2 dephosphorylates phospholipids, important regulators of membrane trafficking, which is a key process in Schwann cells, the glial cells forming myelin in the peripheral nervous system. Our laboratory also generated in vitro and in vivo models of CMT4B1, which have been instrumental over the years to study the pathophysiology of this neuropathy. By investigating why loss of MTMR2 in Schwann cells provokes aberrant myelin, we identified a novel mechanism by which MTMR2 and its lipid substrate coordinate cytoskeleton dynamics and membrane growth within myelin-forming cells. In this project, we will further explore this mechanism of relevance in cell biology. We will also test whether pharmacological and/or genetic modulation of these pathways can represent an effective strategy for the therapy of CMT4B with aberrant myelin.
https://doi.org/10.55762/pc.gr.157015
Grantee: Alessandra Bolino, Ph.D.
Grant type: Research Grant
Award total: $263,450 (Co-funded with CMT Research Foundation)
Institution: San Raffaele Hospital (Ospedale San Raffaele)
Country: Italy
Grantee: Daniel Bittel, Ph.D., D.P.T.
Funded: 9/1/2022 - 8/31/2025
Grant Type: Development Grant
Disease(s): Limb-girdle muscular dystrophies (LGMD)

LGMD2B is a progressive late adolescent onset disease with development of functional limitations in running and climbing stairs within 3 years of diagnosis, and requirement of wheel-chair assistance for mobility within 20 years, on average. These rates of disease progression are hastened by increased physical activity and exercise. The relationship between physical activity, muscle degeneration, and functional mobility deficits in LGMD2B, is thought to derive, in-part, from poor membrane repair and inadequate dysferlin-mediated ASM secretion in response to frequent myofiber membrane injury with activity and exercise. This deficit identifies extracellular ASM supplementation as a potential treatment to improve myofiber repair for LGMD2B and preserve functional mobility. ASM enzyme replacement therapy offers an alternative, but there are currently no approved drugs to address this or other disease etiology of dysferlinopathy. However, liver gene transfer with AAV vectors has successfully treated hemophilia B in humans, by inducing liver expression and secretion of therapeutic concentrations of circulating FIX protein. A similar treatment approach may be leveraged to bypass deficient injury triggered ASM secretion in LGMD2B, by providing myofibers with an increased pool of extracellular ASM for repair, derived from the transduced liver. Optimizing the pre-clinical efficacy and safety of a liver-targeted ASM-AAV treatment in LGMD2B is required for integration into the clinic.
https://doi.org/10.55762/pc.gr.157028
Grantee: Daniel Bittel, Ph.D., D.P.T.
Grant type: Development Grant
Award total: $209,811
Institution: Children's Research Institute (CNMC)
Country: DC, United States
Grantee: Charles Abrams M.D., Ph.D.
Funded: 9/1/2022 - 8/31/2025
Grant Type: Research Grant
Disease(s): Charcot-Marie-Tooth disease (CMT)
Charcot-Marie-Tooth disease (CMT) is a common and debilitating disorder, affecting about 130,00 people in the United States and several million throughout the world and the X-linked form cased by mutations the GJB1 gene is the second most common. With the widespread availability of genetic testing, over 700 variants in GJB1 have been identified. However many of these are likely not disease causing. This leads to great difficulty with advising patients when results of genetic testing are obtained, because there is currently no way to reliably identify which of these variants are disease causing. This proposal aims to address that problem by studying a subset of these not characterized variants to allow us to develop an algorithm for determining pathogenicity of GJB1 variants.
https://doi.org/10.55762/pc.gr.157043
Grantee: Charles Abrams M.D., Ph.D.
Grant type: Research Grant
Award total: $299,865
Institution: The Board of Trustees of the University of Illinois - University of Illinois at Chicago
Country: Illinois, United States
Funded: 9/1/2022 - 8/31/2025
Grant Type: Development Grant
Disease(s): ALS (amyotrophic lateral sclerosis)

A hexanucleotide repeat expansion in the C9ORF72 gene is the most common genetic cause of amyotrophic lateral sclerosis (ALS) and frontotemporal dementia (FTD), two adult-onset progressive neurodegenerative diseases. One of the major hypotheses for toxicity is the accumulation of dipeptide repeat (DPR) proteins produced by RNA repeats. There were many studies unraveling the toxicities by different DPRs. In particular, poly-GR is one of the most toxic DPRs and is found to correlate with neurodegeneration in C9ORF72-related ALS, implicating the contribution of poly-GR to the disease etiology. Therefore, we performed a genetic screening in human neurons to identify modifiers that regulate the poly-GR mediated toxicity. I identified and validated one candidate modifier, knockdown of which strongly improved the survival of the poly-GR expressing neurons. I now propose to further decipher the neuroprotection mechanism, and validate the rescue efficacy in both C9ORF72-ALS patient-derived neurons and the mouse model. This study will provide novel insights on disease mechanisms and potential therapeutic target.
https://doi.org/10.55762/pc.gr.157004
Grantee: Zhe Zhang, Ph.D
Grant type: Development Grant
Award total: $210,000
Institution: Johns Hopkins University School of Medicine
Country: Maryland, United States
Grantee: Armando Villalta, PhD
Funded: 9/1/2022 - 8/31/2024
Grant Type: Research Grant
Disease(s): Duchenne muscular dystrophy (DMD), Becker muscular dystrophy (BMD)

In some Duchenne muscular dystrophy (DMD) patients the development of transgene-specific immunity raises safety concerns and the need for novel approaches to study and mitigate these unwanted immune responses. The recognition of dystrophin-expressing muscle cells by dystrophin-specific T cells may result in the rejection of muscle cells that express dystrophin. Our studies will explore a new approach to re-educate the DMD patient's immune system to understand that it should not mount a response to the dystrophin protein that is expressed after gene therapy. To achieve this, we will use regulatory T cells (Tregs), which normally instruct the immune system to not attack self-proteins. We will engineer a muscle-specific Treg that will be used to inhibit the activation of dystrophin-specific T cells in a novel mouse model of dystrophin immunity our lab developed. Muscle-specific Tregs, thus represent a novel approach for addressing the recent observation in dystrophin gene therapy trails that SAEs are partly attributed to dystrophin-specific T cells, and have great potential for transforming the approaches used to inhibit immunological responses to gene therapy in DMD patients.
https://doi.org/10.55762/pc.gr.157011
Grantee: Armando Villalta, PhD
Grant type: Research Grant
Award total: $200,000
Institution: The Regents of the University of California (Irvine)
Country: California, United States
Grantee: Emilie Venereau, Ph.D
Funded: 9/1/2022 - 8/31/2025
Grant Type: Research Grant
Disease(s): Duchenne muscular dystrophy (DMD), Becker muscular dystrophy (BMD)
Muscular dystrophies are a family of genetic diseases characterized by progressive muscle degeneration. Duchenne muscular dystrophy is the most common and lethal muscle-wasting disease of childhood, which is still incurable. Pharmacological corticosteroid therapy is the standard of care for patients affected by Duchenne muscular dystrophy to control symptoms and slow disease progression through potent anti-inflammatory action. However, these current treatments have limited efficiency and a major concern is the significant adverse effects associated with long term-treatment. In our laboratory, we study a protein, called HMGB1, which is a key player in inflammatory and regenerative processes. We generated a designer HMGB1 protein devoid of inflammatory activity but endowed with potent regenerative properties in muscle. We recently demonstrated that administration of our designer protein stimulates regeneration and ameliorates the muscle function, aside from reducing degeneration, inflammation, and fibrosis, in mouse models of muscular dystrophies. Our objective is to conduct a preclinical evaluation of this novel molecule as drug candidate for patients affected by Duchenne muscular dystrophy. Hence, our study is oriented towards a translational approach to develop an innovative therapeutic strategy for patients affected by Duchenne muscular dystrophy and preliminary data indicate that in future, these results might be extended to other forms of muscular dystrophy.
https://doi.org/10.55762/pc.gr.157017
Grantee: Emilie Venereau, Ph.D
Grant type: Research Grant
Award total: $300,000
Institution: San Raffaele Hospital (Ospedale San Raffaele)
Country: Italy
Grantee: Paul Valdmanis, Ph.D
Funded: 9/1/2022 - 8/31/2025
Grant Type: Research Grant
Disease(s): ALS (amyotrophic lateral sclerosis)
The number of people in our world over 60 years old is estimated to more than double by 2050. As life expectancy increases, so will the prevalence of age-related neurodegenerative diseases including Amyotrophic Lateral Sclerosis (ALS). The genetic contributions that lead to ALS are still not fully clear despite intensive sequencing efforts, necessitating further studies into genes that cause or modify ALS. We hypothesize that a significant genetic contribution to disease comes from regions of the human genome that are still challenging to characterize using standard sequencing technology. Some of these regions contain repetitive stretches of DNA can expand in patient populations and often can manifest in different neurodegenerative disorders. We have established techniques to characterize these genetic regions in a multiplexed high-throughput manner. We propose to use our approaches to determine the contributions of these repeats to ALS, determine how they aggregate in cells and what additional factors they can bring into these aggregates. Our proposed work will provide insight into novel mechanisms of ALS and help bridge genes associated with disease for the purpose of devising novel therapeutics.
https://doi.org/10.55762/pc.gr.157016
Grantee: Paul Valdmanis, Ph.D
Grant type: Research Grant
Award total: $300,000
Institution: University of Washington
Country: Washington, United States
Grantee: Martine Therrien, Ph.D
Funded: 9/1/2022 - 9/1/2025
Grant Type: Development Grant
Disease(s): ALS (amyotrophic lateral sclerosis)

Although most therapeutic avenues for Amyotrophic lateral sclerosis (ALS) have focused on neurons, recent studies suggest that microglia, the immune cells of the brain, are key players in pathogenesis, pointing toward alternative approaches to therapeutic development. Many genetic risk factors for ALS are expressed in microglia and recently, a distinct subpopulation, or “state”, has been identified in ALS patients. Interestingly, microglia have also been involved in other neurodegenerative diseases like Alzheimer’s disease. In this study, we used human cell culture models and single-cell-resolution analyses to identify how ALS genetics affect microglia states and functions and understand how microglia affect motor neuron health. This project will identify pathways of neurodegeneration specific to ALS and open the door for new therapeutic avenues.
https://doi.org/10.55762/pc.gr.156998
Grantee: Martine Therrien, Ph.D
Grant type: Development Grant
Award total: $208,027
Institution: Broad Institute (Eli and Edythe L. Broad Institute of MIT and Harvard)
Country: Massachusetts, United States
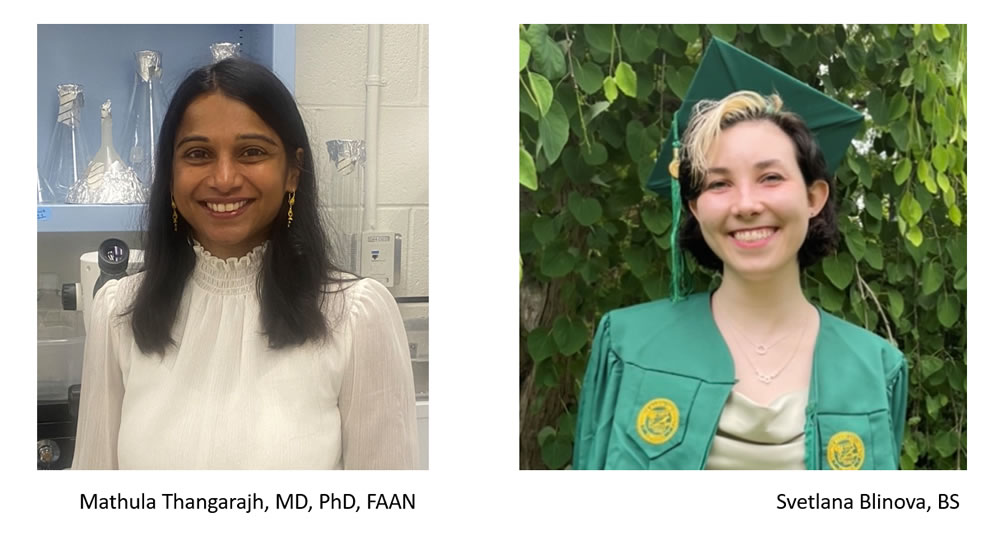
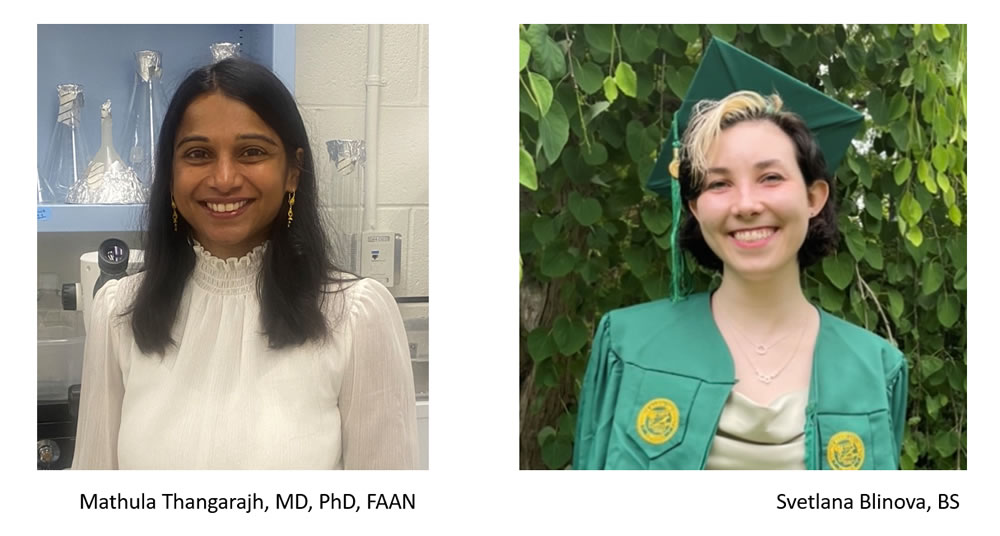
Grantee: Mathula Thangarajh, PhD
Funded: 9/1/2022 - 8/31/2023
Disease(s): Duchenne muscular dystrophy (DMD), Becker muscular dystrophy (BMD)
Duchenne Muscular Dystrophy (DMD) is more than just a muscle disease. Boys with DMD have a distinct cognitive profile including lower intelligence quotient, executive function problems, working memory deficits, communication and language difficulties. Second to the muscle, the highest expression of dystrophin protein is in the central nervous system underscoring the importance of dystrophin in neuronal and glial function. To more deeply understand the role of dystrophin in hippocampal neurons, it is imperative to delve deeply into the molecular mechanisms that go awry. Towards this goal, we will use the preclinical mouse model of DMD, the mdx52 mouse, and a cutting-edge technique -- single nuclei RNA sequencing -- to specify the neuronal transcriptome. This knowledge has two immediate outcomes. First, we will have a detailed account of neuronal transcriptome. Second, using this knowledge, we would be able to identify what genetic pathways are abnormal so we can design mechanistically-driven therapeutic agents. This MDA Idea Development Award will offset cost for the single nuclei RNA sequencing.
https://doi.org/10.55762/pc.gr.157053
Grantee: Mathula Thangarajh, PhD
Grant type: Idea Award
Award total: $50,000
Institution: Virginia Commonwealth University
Country: Virginia, United States
Grantee: Mathula Thangarajh, PhD
Funded: 9/1/2022 - 12/31/2023
Grant Type: Clinical Trial Travel Grant
Disease(s): Duchenne muscular dystrophy (DMD), Becker muscular dystrophy (BMD)
In recent years, health disparities in accessing health and opportunities to clinical trials have emerged as critical unmet needs not only in the general population but also in rare diseases. Barriers to equitable access to healthcare opportunities includes difficulty accessing information, geographic location, financial burden due to work productivity loss. Our prior research knowledge and experience has demonstrated that mitigating financial burden can be a powerful incentive for families to consider participation in clinical research. We will advance this approach using our recently funded R21 award to investigate a technology-enabled platform to assess cognition in dystrophinopathy. This application will serve to support travel and travel-related costs, so that families and research participants, regardless of socioeconomic status and geographic location will have equitable access to our study.
https://doi.org/10.55762/pc.gr.156495
Grantee: Mathula Thangarajh, PhD
Grant type: Clinical Trial Travel Grant
Award total: $69,460
Institution: Virginia Commonwealth University
Country: Virginia, United States
Grantee: Tyler Tarr, Ph.D.
Funded: 9/1/2022 - 8/31/2025
Grant Type: Development Grant
Disease(s): Lambert-Eaton myasthenic syndrome (LEMS)

Many neuromuscular diseases result in functional disruptions at the neuromuscular junction (NMJ); the site of communication between motor neurons and muscle fibers. Lambert-Eaton Myasthenic Syndrome (LEMS) is caused when a patient’s own immune system attacks and removes calcium channels from transmitter release sites at the NMJ, causing muscle weakness. Previously, the simple loss of calcium channels was thought to result in the muscle weakness seen in LEMS, but recently it has become apparent that the pathophysiology of LEMS is more complicated. In fact, the organization of many proteins at the neurotransmitter release site is significantly disrupted in LEMS, indicating a more complex pathophysiology. Unfortunately, exploring the specific proteins whose organization is disrupted in LEMS has not been possible because of the technical limitations of imaging these very small regions of the NMJ. However, recent advances in super-resolution microscopy can now provide the resolution necessary to observe the changes that occur at transmitter release sites in LEMS. This proposal aims to identify the specific proteins that are altered in LEMS, which will provide new potential targets for the development of alternative therapies. The data generated from this project will also enhance our understanding of neurotransmitter release sites at the NMJ, which may prove beneficial for the development of treatments for other neuromuscular diseases.
https://doi.org/10.55762/pc.gr.156997
Grantee: Tyler Tarr, Ph.D.
Grant type: Development Grant
Award total: $208,212
Institution: University of Pittsburgh
Country: Pennsylvania, United States
Grantee: Amirhossein Taghavi, PhD
Funded: 9/1/2022 - 8/31/2025
Grant Type: Development Grant
Disease(s): Myotonic dystrophy (DM)

Repeat expansions are a class of disease causing RNAs causing more than 30 different diseases including myotonic dystrophy type 1 (DM1). These disease causing RNA molecules have structured regions with biological functionality. In a structure based approach, small molecules, can target these structured regions, called binding pocket. DM1 is caused by an expanded CTG repeat. After being transcribed into RNA this expanded repeat forms a hairpin structure with multiple repeating 1x1 UU internal loops. These internal loops provide a high affinity binding pocket for proteins like muscleblind-like 1 (MBNL1) and sequester them in nuclear foci. Small molecules with high binding affinity toward these binding pockets can either liberate MBNL1 or inhibit its interaction with the binding pocket and restore the MBNL1 activity. Finding small molecules with high binding affinity toward the binding pocket is the first and most challenging step in the process of restoring MBNL1 activity and therefore alleviating the DM associated defects. Virtual screening approaches such as docking and 2D fingerprint similarity searches provide the opportunity to screen millions of small molecules, identifying the lead compounds with highest affinity toward the binding pocket. Lead compounds found through these approaches will then be subject to a barrage of experimental studies for their selectivity and potency in DM1 cellular models including patient derived cells.
https://doi.org/10.55762/pc.gr.157023
Grantee: Amirhossein Taghavi, PhD
Grant type: Development Grant
Award total: $210,000
Institution: University of Florida
Country: Florida, United States
Grantee: Charlotte Sumner, M.D.
Funded: 9/1/2022 - 8/31/2025
Grant Type: Research Grant
Disease(s): Spinal muscular atrophy (SMA)

New gene targeting treatments that increase survival motor neuron (SMN) protein expression can substantially improve motor function in spinal muscular atrophy (SMA) patients when given before disease onset, but have modest effects when given post-symptomatically. Unfortunately emerging data indicates that for the most common and severe SMA type I, precipitous motor axon neurodegeneration is ongoing neonatally. We postulate that temporarily halting axonal degeneration could enhance the efficacy of SMN induction therapeutics. The sterile-a and Toll/interleukin 1 receptor (TIR) motif containing protein 1 (SARM1) is a NADase that triggers motor axon degeneration. Our preliminary data indicate that genetic knock out of SARM1 is associated with prevention of proximal motor axon loss neonatally in SMA mice. In this study, we will assess the durability of this effect and the therapeutic potential of SARM1 inhibition together with SMN induction in severe SMA mice. These studies will provide proof of concept to support the development of a novel combinatorial treatment for SMA patients.
https://doi.org/10.55762/pc.gr.157037
Grantee: Charlotte Sumner, M.D.
Grant type: Research Grant
Award total: $300,000
Institution: Johns Hopkins University School of Medicine
Country: Maryland, United States
Grantee: Erik Storkebaum, Ph.D.
Funded: 9/1/2022 - 8/31/2025
Grant Type: Research Grant
Disease(s): Charcot-Marie-Tooth disease (CMT)

Unravelling the molecular mechanism underlying an incurable disease Charcot-Marie-Tooth (CMT) is an incurable disease in which motor and sensory nerves degenerate, leading to muscle weakness and sensory deficits. CMT is a genetic disease, and changes in many different genes can cause CMT. It is incompletely understood how these changes in CMT genes ultimately result in degeneration of motor and sensory nerves. Currently, no effective drug treatment is available for any genetic form of CMT. Among the CMT genes, mutations in 6 distinct genes that produce so-called ‘transfer RNA (tRNA) synthetases’ cause CMT. Scientists recently elucidated a novel mechanism that underlies CMT caused by mutations in one of these tRNA synthetases, the glycyl-tRNA synthetase. Now, they wish to evaluate whether a similar mechanism applies to CMT caused by mutations in the other tRNA synthetase genes. If so, this would imply that administration of tRNA may constitute a novel therapeutic approach for these incurable diseases.
Image Source: Prinses Beatrix Spierfonds
https://doi.org/10.55762/pc.gr.157000
Grantee: Erik Storkebaum, Ph.D.
Grant type: Research Grant
Award total: $300,000
Institution: Stichting Radboud Universiteit
Country: Netherlands
Grantee: Jeffrey Statland, M.D.
Funded: 9/1/2022 - 8/31/2026
Grant Type: Clinical Research Network Grant
Disease(s): Facioscapulohumeral muscular dystrophy (FSHD)

Advances in our understanding of muscular dystrophies (MDs) have identified targets for treatment for facioscapulohumeral muscular dystrophy, myotonic dystrophy, and limb girdle muscular dystrophy. Indeed, several clinical trials of new gene targeted drugs are underway for each MD. Despite that, companies have identified several barriers to drug development including the need for biomarkers, outcome measures to support drug registration, and standardized site training to prepare for clinical trials. We formed clinical trial research networks to hasten therapeutic development for many of the MDs. In the current proposal, we plan to consolidate the project management and oversite of the research networks into a single MD Clinical Trial Research Network. This network of 15 core United States centers brings together national leaders in MD research, sets the stage for common site training and patient engagement, and allows for us to also advance patient care, by providing training and online resources related to MD. Such a research network can work with patients and their family members, industry, academics, and drug companies to overcome lingering barriers to drug development, including trial preparedness studies to validate better biomarkers and clinical outcome assessments for drug approval. Finally, by having such a large national effort we can train the next generation of MD researchers, to ensure continuity and excellence in care in the future.
Funded in collaboration with LGMD2i Research Fund and CureLGMD2i Foundation
https://doi.org/10.55762/pc.gr.157025
Grantee: Jeffrey Statland, M.D.
Grant type: Clinical Research Network Grant
Award total: $1,517,502
Institution: University of Kansas Medical Center Research Institute, Inc
Country: Kansas, United States
Grantee: Nandhini Sivakumar, Ph.D.
Funded: 9/1/2022 - 8/31/2025
Grant Type: Development Grant
Disease(s): Spinal muscular atrophy (SMA)

Movement and muscle control are regulated by the activity of motor neurons which are located in the spinal cord. Spinal motor neurons convey central commands to their peripheral targets, the skeletal muscles. Pre-motor neurons make synaptic contacts with motor neurons and regulate their function. However, the molecular mechanisms underlying synaptic-mediated motor neuron function are unknown. To address this, we use in vivo and in vitro models of spinal muscular atrophy a neurodegenerative disease caused by deficiency of the ubiquitously expressed SMN protein. Proximal muscles are preferentially affected during the progression of this disease, compared to more distal muscles. In our proposal, we aim to investigate enzymatic effects on the molecular and cellular function of potassium channels expressed on the motor neurons. Potassium channels are essential to elicit repetitive firing of motor neurons and subsequent muscle contraction. Utilizing enzyme inhibitors that regulate the activity of potassium channels, we aim to uncover the cascade of molecular events leading to the enhancement of motor neuron function. Our study has the potential to reveal salient principles in the restoration of neuronal function in spinal muscular atrophy and offer novel therapeutic avenues.
https://doi.org/10.55762/pc.gr.157009
Grantee: Nandhini Sivakumar, Ph.D.
Grant type: Development Grant
Award total: $210,000
Institution: Columbia University Medical Center
Country: New York, United States
Grantee: Michael Shy, M.D.
Funded: 9/1/2022 - 8/31/2025
Grant Type: Infrastructure Grant
Disease(s): Charcot-Marie-Tooth disease (CMT)
The Inherited Neuropathy Consortium is dedicated to developing the infrastructure necessary to evaluate therapies for patients with Charcot-Marie-Tooth disease. We have developed CMT specific clinical outcome assessments to measure the effects of CMT on adults and children. We have identified markers of disease severity in blood, from skin biopsies and also by MRI imaging of muscles. We have had a Critical Path Innovation Meeting with the FDA on how best to use our measures to bring successful clinical trials to our patient population. Developing rational therapies for patients requires knowing the cause of their CMT. We have identified 23 novel genetic causes of CMT. We have initiated the CMT Variant Browser which promotes sharing of genetic information on CMT for patients, their families, caregivers and researchers. We have successfully trained 14 young investigators to carry on future CMT research, many of whom have obtained faculty positions in fields related to CMT. We are applying to continue MDA support through 2024 which coincides with the end of our currently funded NIH five year cycle to continue natural history studies with various CMT subtypes, continue gene identification and genetic modifier studies using whole genome sequencing, develop the use of remote evaluations of patients and train future investigators.
https://doi.org/10.55762/pc.gr.157060
Grantee: Michael Shy, M.D.
Grant type: Infrastructure Grant
Award total: $439,250
Institution: The University of Iowa
Country: Iowa, United States
Grantee: Joshua Selsby, Ph.D.
Funded: 9/1/2022 - 8/31/2025
Grant Type: Research Grant
Disease(s): Duchenne muscular dystrophy (DMD), Becker muscular dystrophy (BMD)
Obesity and insulin resistance (IR) commonly accompany dystrophin deficiency; however, how they potentiate disease progression and severity is unknown. Indeed, dystrophin deficiency and obesity/IR cause a host of cellular dysfunctions that in some cases overlap and in some cases are distinct. This raises the likelihood of additive and even synergistic effects. Further, glucocorticoids are commonly prescribed to boys with DMD but may also alter cellular metabolism particularly in the case of obesity/IR. To address this gap in knowledge, we will measure muscle function parameters in lean and obese healthy mice and mice with DMD, with or without glucocorticoid treatment. We will also investigate how obesity alters dystrophic metabolism and assess glucose transport, mitochondrial function, and the metabolome and proteome of these mice. We expect to discover that obesity/IR further erodes muscle function and antagonizes muscle metabolic function. This work will provide important information about disease progression in humans as well as about nutritional management of boys with DMD. Further, as the commonly used DMD mouse model, the mdx mouse, is quite lean, outcomes may also improve the utility and predictive power of mdx mice. This would enable treatment strategies to be tested in a physiological and metabolic context that more closely resembles that of humans with DMD.
https://doi.org/10.55762/pc.gr.157040
Grantee: Joshua Selsby, Ph.D.
Grant type: Research Grant
Award total: $300,000
Institution: Iowa State University of Science and Technology
Country: Iowa, United States
Grantee: Markus Ruegg, Ph.D.
Funded: 9/1/2022 - 8/31/2025
Grant Type: Research Grant
Disease(s): Congenital muscular dystrophies (CMD)

Extracellular matrix (ECM) acts as scaffold to provide essential structural support to the surrounding cells. Laminins are essential components of the ECM connecting it tightly with the underlying cell layer, just like the binds between scaffolding and a building. Mutations in this protein family cause a range of severe disorders that affect different organs. The rope-like laminin-211 protein, composed of three intertwined laminin chains, is the main isoform in skeletal muscle. Mutations in the LAMA2 gene, encoding one of the chains in laminin-211, leads to its loss and causes a rare, severe and early-onset muscular dystrophy, called MDC1A or LAMA2 MD. Affected children show muscle wasting and weakness and eventually die from respiratory insufficiency. There is no treatment for LAMA2 MD. We have shown that two specifically designed linker proteins strongly improve the pathology and lifespan in LAMA2 MD mice, which lack laminin-211 like LAMA2 MD patients and display very similar symptoms. In ongoing research, we are developing a gene therapy approach to deliver the two linkers to LAMA2 MD mice by using an adeno-associated viral vector (AAV9). Our initial results show that this gene therapy approach is indeed possible. We now aim to optimize linker delivery using newly developed AAV9 variants (myotropic AAVs) that are even more efficient at infecting skeletal muscles. We are hopeful these experiments will pave the way to a gene therapy treatment for LAMA2 MD patients.
https://doi.org/10.55762/pc.gr.157038
Grantee: Markus Ruegg, Ph.D.
Grant type: Research Grant
Award total: $293,810
Institution: University of Basel (Universität Basel)
Country: Switzerland
Grantee: Michael Rudnicki, PhD
Funded: 9/1/2022 - 8/31/2025
Grant Type: Research Grant
Disease(s): Duchenne muscular dystrophy (DMD), Becker muscular dystrophy (BMD)

Duchenne Muscular Dystrophy (DMD) is a muscle wasting disease that leads to premature death. We discovered that muscle stem cells in DMD are defective and regeneration is unable to keep pace with the muscle damage. We have developed a drug that overcomes this deficit and observed that treated DMD mice show a large improvement in muscle function. We will determine the optimal dose that promotes the best response without adverse effects, we will evaluate the efficacy of long-term treatment in preventing disease progression, and we will evaluate whether drug stimulation of regeneration can repair existing dystrophic damage. We will treat mice with drug and gene therapy to evaluate combination therapy. Finally, we will validate that the drug works the same in human muscle tissue. Together, these experiments will provide important proof-of-concept data that a drug that stimulates muscle regeneration is potentially effective as a treatment for DMD.
https://doi.org/10.55762/pc.gr.156999
Grantee: Michael Rudnicki, PhD
Grant type: Research Grant
Award total: $300,000
Institution: Ottawa Hospital Research Institute
Country: Ontario, Canada
Grantee: Fabio Rossi, M.D., Ph.D.
Funded: 9/1/2022 - 8/31/2025
Grant Type: Research Grant
Disease(s): Duchenne muscular dystrophy (DMD), Becker muscular dystrophy (BMD)

The standard of care for Duchenne Muscular Dystrophy (DMD) includes corticosteroids that, while partially effective at delaying disease progression, are associated with significant side effects, due to which they often need to be interrupted. Despite therapeutic interventions, patients with DMD become wheelchair bound during adolescence and by early adulthood they need assistance for eating and drinking and require assisted ventilation. Therefore, the identification of safer alternative therapies, or therapies that would cooperatively enhance the effect of corticosteroids would greatly benefit DMD patients. Our recent findings in a mouse model of DMD suggests that CSF1R inhibitors, a class of drugs recently approved by The United States Food and Drug Administration (FDA) as anti-cancers in human patients, have the potentials to reduce muscle damage in DMD. Here, we propose a preclinical trial of a CSF1R inhibitor in dystrophic rats, a newly developed animal model that better represents human DMD. We will assess the efficacy of this drug by itself, as well as in the context of current standard therapies given to DMD patients. This is a prerequisite to engage the regulatory path leading to clinical trials in human patients.
https://doi.org/10.55762/pc.gr.157019
Grantee: Fabio Rossi, M.D., Ph.D.
Grant type: Research Grant
Award total: $300,000
Institution: University of British Columbia
Country: British Columbia, Canada
Grantee: George Rodney, Ph.D.
Funded: 9/1/2022 - 8/31/2025
Grant Type: Research Grant
Disease(s): Duchenne muscular dystrophy (DMD), Becker muscular dystrophy (BMD)

It is clear that exposures to cannabidiol (CBD) are increasing. It is also clear that CBD possesses therapeutic benefit, and in some cases, the beneficial effects of CBD are for diseases for which other available treatments have not been efficacious. The new perspective is to combine different therapeutic approaches to improve the efficacy of the single treatment, CBD combined with current steroid treatment may improve the anti-inflammatory effects of those therapies. These observations suggest that CBD has potential and there is a critical need to assess the efficacy of CBD in improving skeletal muscle function, pulmonary function, and immunological function in DMD.
https://doi.org/10.55762/pc.gr.157021
Grantee: George Rodney, Ph.D.
Grant type: Research Grant
Award total: $300,000
Institution: Baylor College of Medicine
Country: Texas, United States
Grantee: David Richman, M.D.
Funded: 9/1/2022 - 8/31/2025
Grant Type: Research Grant
Disease(s): Myasthenia gravis (MG)
Myasthenia gravis (MG) is an autoimmune (AI) disease, i.e., disorders in which control of the immune system becomes dysfunctional, allowing production of antibodies (Abs) that attack the body itself. In MG the target of AI attack is the crucial connection between nerve and muscle, which leads to the muscle weakness that characterizes the disease. Currently available treatments of AI diseases in general, and MG in particular, involve drugs that nonspecifically reduce the activity of the entire immune system, both the abnormal AI portions and the normally functioning portions. Use of these agents requires balancing the disease-directed effect with the side effects resulting from nonspecific blockade of normal immune function. The current project aims at developing a treatment for MG (and possibly other AI diseases) that affects only the abnormal AI portion of the immune system by targeting the production of the abnormal Abs directed at the nerve-muscle connection. Some of the patient’s immune cells (T cells) will be engineered to attack the subset of Ab-generating cells (B cells) that produce the AI Abs, leaving all other B cells untouched. This is possible because each B cell displays on its surface the single Ab it is capable of making. The engineered T cells target the AI Abs on the surface of the abnormal B cells, stopping the production of the auto-Abs, potentially terminating the disease – while leaving the rest of the immune system intact.
https://doi.org/10.55762/pc.gr.157005
Grantee: David Richman, M.D.
Grant type: Research Grant
Award total: $300,000
Institution: The Regents of the University of California (University of California Davis)
Country: California, United States
Funded: 9/1/2022 - 8/31/2025
Grant Type: Research Grant
Disease(s): Duchenne muscular dystrophy (DMD), Becker muscular dystrophy (BMD)
We propose to develop a novel form of gene therapy for Duchenne muscular dystrophy which will have greater durability and broader applicability than therapies currently in clinical trials. Our approach would enable neonatal or even fetal gene therapy, and would eliminate the risk of gradual loss of efficacy that might complicate standard gene therapy approaches. We will test our novel gene therapy for safety and efficacy in mice with Duchenne muscular dystrophy, and look for potential problems caused by modification of the genome.
https://doi.org/10.55762/pc.gr.157045
Grantee: William Pu, MD
Grant type: Research Grant
Award total: $299,979
Institution: Boston Children's Hospital
Country: Massachusetts, United States
Grantee: Jae Mo Park, PhD
Funded: 9/1/2022 - 8/31/2023
Disease(s): Mitochondrial myopathies, Encephalomyopathies

Duchenne muscular dystrophy (DMD) and Becker muscular dystrophy (BMD) are the most common types of neuromuscular diseases that are resulted from mutations in the dystrophin genes. Patients develop progressive muscle weakness and atrophy, and most of them die of heart failure. Currently, there is no cure for the diseases and no standard method for monitoring the disease progression. Muscular dystrophy is accompanied by apparent metabolic alterations such as tissue inflammation and mitochondrial dysfunction. These metabolic shifts typically precede development of muscular atrophy and have potentials to be developed as early biomarkers for muscular dystrophy. In this proposed study, we will develop in-vivo biomarkers for inflammation and mitochondrial dysfunction in muscular dystrophy using a quick (few minutes), safe, and powerful metabolic imaging method. The method, so-called ‘hyperpolarized 13C MRI’, uses a bolus injection of pyruvate, a natural metabolite, and has been already tested with more than 200 injections in healthy volunteers and patients at UT Southwestern without having any adverse effects over the last few years. In this study, we will recruit patients with DMD or BMD, and acquire metabolic images of the heart and the skeletal muscle during a single MRI session. In the future, these tools may help identify the start of heart failure, develop therapeutic targets, or detect early metabolic response to therapy.
https://doi.org/10.55762/pc.gr.157052
Grantee: Jae Mo Park, PhD
Grant type: Idea Award
Award total: $50,000
Institution: The University of Texas Southwestern Medical Center (UT Southwestern)
Country: Texas, United States
Grantee: James Novak, Ph.D.
Funded: 9/1/2022 - 8/31/2023
Disease(s): Duchenne muscular dystrophy (DMD), Becker muscular dystrophy (BMD)

Mutations in dystrophin gene leads to Duchenne muscular dystrophy (DMD). Use of exon skipping antisense oligonucleotide (AO) drugs designed to skip over the mutations in the dystrophin gene helps express a shorter version of the dystrophin protein, helping reduce muscle pathology in the DMD patients. Despite the great potential of AO drugs for DMD and other neuromuscular diseases, their clinical expectations for DMD have not been met due to the inefficient delivery of these drugs to skeletal and cardiac muscle. The work presented here aims to address this bottleneck, through an approach that encapsulates AO within lipid nanoparticles (LNP). This enhances drug bioavailability in the bloodstream and within the muscle tissue, allowing for greatly reduced drug loads as compared to current AO dosing strategies. Investigations proposed here will build on these features of LNPs by harnessing the potential of LNP encapsulated AOs to improve delivery and retention of these drugs, leading to their enhanced efficacy for DMD therapy.
https://doi.org/10.55762/pc.gr.157049
Grantee: James Novak, Ph.D.
Grant type: Idea Award
Award total: $50,000
Institution: Children's Research Institute (CNMC)
Country: DC, United States
Grantee: Peter Noakes, Ph.D.
Funded: 9/1/2022 - 8/31/2025
Grant Type: Research Grant
Disease(s): Duchenne muscular dystrophy (DMD), Becker muscular dystrophy (BMD)

Healthcare providers routinely prescribe glucocorticoid steroids to help control the symptoms of DMD. However, there are an inherent number of significant side effects associated with long-term steroid use leading to dose reduction or suspension and ultimately decreased efficacy. It is well recognized that new treatments for DMD with better safety and efficacy profiles are required. We have developed several potent and selective drug compounds that block a key inflammatory pathway, one of which has been shown to reduce muscle damage in mouse models of DMD. We aim to optimize our candidate compounds in pre-clinical testing in animal models of DMD, so as to progress our best lead drug compound towards human clinical trials. Our proposed pre-clinical experiments in DMD model mice (mdx mice) will generate the required data to guide selection of a preferred candidate that will ultimately be taken forward to Investigational New Drug (IND) enabling studies and into the clinic.
https://doi.org/10.55762/pc.gr.157039
Grantee: Peter Noakes, Ph.D.
Grant type: Research Grant
Award total: $293,667.27
Institution: University of Queensland (UQ)
Country: Australia
Grantee: Chiara Mozzetta, Ph.D.
Funded: 10/1/2022 - 9/30/2025
Grant Type: Research Grant
Disease(s): Emery-Dreifuss muscular dystrophy (EDMD)

Our project focuses on fibro-adipogenic progenitors (FAPs), a population of muscle-resident cells that support the formation of new muscle during skeletal muscle regeneration but also give rise to fibrotic and fat cells that accumulate in degenerating muscles. We aim here to study whether this population of cells plays a pathogenic role in Emery-Dreifuss Muscular Dystrophy, a rare genetic muscle disease caused by mutation in a gene encoding for Lamin A/C a protein that resides in the nuclear envelope. In particular, our goal is to understand how mutations in Lamin A/C affect the capacity of FAPs to differentiate into fibrotic and fat cells by studying whether their genome is re-configured in the absence of a functional Lamin A/C. Our ultimate objective is to find new therapeutic cellular targets to develop strategies to block the loss of muscle tissue and the formation of fat and fibrotic scars in EDMD muscles.
https://doi.org/10.55762/pc.gr.157036
Grantee: Chiara Mozzetta, Ph.D.
Grant type: Research Grant
Award total: $279,300
Institution: CNR-Institute of Molecular Biology and Pathology
Country: Italy
Grantee: Carlos Moraes, Ph.D.
Funded: 9/1/2022 - 8/31/2025
Grant Type: Research Grant
Disease(s): Mitochondrial myopathies, Encephalomyopathies
Mitochondrial DNA deletions are a relatively common cause of myopathy among the mitochondrial diseases population. We have generated tools to eliminate mtDNA deletions, but have not been able to test them in vivo because no mammalian models exist. Here we propose to develop a mouse model with high levels of mtDNA deletions and treat these mutant molecules with DNA editing enzymes. We will also explore non-viral delivery system of these enzymes to muscle and liver.
https://doi.org/10.55762/pc.gr.157044
Grantee: Carlos Moraes, Ph.D.
Grant type: Research Grant
Award total: $300,000
Institution: Miller School of Medicine of the University of Miami
Country: Florida, United States
Grantee: Brett McCray MD., Ph.D
Funded: 9/1/2022 - 8/31/2025
Grant Type: Clinical Research Grant
Disease(s): Charcot-Marie-Tooth disease (CMT)
Charcot-Marie-Tooth disease (CMT) includes a group of inherited peripheral neuropathies that cause symptoms of progressive weakness and loss of sensation. CMT is the most common inherited neurological condition worldwide, but there are currently no available treatments to slow progression of any forms of this disease. A subtype of CMT, known as CMT type 2C, is caused by mutations in TRPV4, which is an ion channel that can open or close to allow calcium to enter cells. Our work in animal models of this condition has shown that disease mutations in TRPV4 cause the channel to be overactive, and drugs that block the channel are highly effective as treatments in these animal models. This suggests that available TRPV4 blocking drugs are a promising potential treatment for patients with TRPV4 mutations. However, there are still important barriers that need to be overcome in order to facilitate a clinical trial for this condition. In particular, the natural progression of CMT2C and readouts of disease progression must be better defined to determine the specific outcome measures that would be used in a clinical trial. This proposal will use a comprehensive clinical approach to define markers of disease severity and progression in patients, an essential step in the process of moving towards a clinical trial and ultimately establishing a treatment for CMT2C. If successful, this would be a ground-breaking accomplishment and pave the way for clinical trials for other forms CMT.
https://doi.org/10.55762/pc.gr.157002
Grantee: Brett McCray MD., Ph.D
Grant type: Clinical Research Grant
Award total: $497,011
Institution: Johns Hopkins University School of Medicine
Country: Maryland, United States
Grantee: Gordon Lynch, Ph.D.
Funded: 9/1/2022 - 8/31/2025
Grant Type: Research Grant
Disease(s): Duchenne muscular dystrophy (DMD), Becker muscular dystrophy (BMD)

Although micro-dystrophin gene therapy offers promise as a treatment for DMD, the current lack of full gene correction means shortcomings in addressing all aspects of the pathology. For DMD, counteracting wasting and weakness and improving the pathology requires a strategy that ideally produces larger (and stronger) muscles, without causing fatigue, and protects them from injury. This requires simultaneously manipulating signaling pathways that promote hypertrophy and oxidative metabolism. Although exercise has many health benefits for improving muscle strength and endurance, most DMD patients cannot exercise. A solution may come from ‘exercise mimetics’ that can confer exercise-like improvements in muscle structure, function, and metabolism. Powerful pharmacologics are available that can alter muscle phenotype; beta-agonists (like formoterol), can promote muscle mass and strength; and adenosine monophosphate-activated protein kinase (AMPK) activators (like MK-8722), can enhance oxidative metabolism. This proposal will interrogate the therapeutic potential of simultaneously manipulating growth and oxidative metabolism through a combined formoterol-MK-8722 strategy, with potential to confer improvements in muscle function without compromising metabolism or injury susceptibility. If successful, this would represent a novel repurposing of approved drugs as a treatment for DMD and provide strong support for this novel adjuvant combination to be advanced to the clinic.
https://doi.org/10.55762/pc.gr.157018
Grantee: Gordon Lynch, Ph.D.
Grant type: Research Grant
Award total: $299,872.32
Institution: University of Melbourne (Melbourne University)
Country: Australia
Grantee: John Lueck, Ph.D.
Funded: 9/1/2022 - 8/31/2025
Grant Type: Research Grant
Disease(s): Myotonic dystrophy (DM)

DM1 is an autosomal dominant disease characterized by muscle weakness and myotonia, often leading to premature death from respiratory failure. Presently there is no treatment to reverse or slow the progressive decline. DM1 is caused by expansion of a CTG repeat in the 3’ untranslated region of DMPK. The repeat expansion containing RNA expressed, exhibits a toxic gain-of-function that results in misregulated alternative splicing of specific transcripts and the inappropriate expression of neonatal transcript isoforms in mature muscle. DM1 is estimated to affect >100,000 people in the U.S. alone, many of whom experience decades of progressive disability. Our preliminary results demonstrate that oral feeding of an already FDA approved voltage-gated calcium channel drug significantly rescues phenotypes and extends the lifespan of a reductionist DM1 mouse model with targeted missplicing events. Here we will use a RNA toxicity DM1 mouse that models severe DM1 myopathic features, including the full spectrum of aberrant splice events, and shortened lifespan. We will target the muscle voltage-gated calcium channel in two ways to determine its role in DM1 pathophysiology and provide proof-of-concept for repurposing an FDA approved drug for treatment of DM1 for rapid transition into the clinic.
https://doi.org/10.55762/pc.gr.157033
Grantee: John Lueck, Ph.D.
Grant type: Research Grant
Award total: $300,000
Institution: University of Rochester
Country: New York, United States
Grantee: Rashmi Kothary, Ph.D.
Funded: 9/1/2022 - 8/31/2025
Grant Type: Research Grant
Disease(s): Spinal muscular atrophy (SMA)

Our laboratory has been at the leading edge in the identification of non-neuronal defects in spinal muscular atrophy (SMA). We have shown that SMN depletion leads to defects in fatty acid metabolism. This novel finding raises the intriguing question of whether liver metabolic alterations are an important facet of SMA disease pathogenesis. Here we will perform a more in-depth investigation to examine fatty acid metabolism in SMA. The proposed experiments will address the triggering events in liver steatosis in SMA and whether the liver is an important player in the overall picture of SMA disease etiology. The research will have important implications in the care and disease management of patients with SMA.
https://doi.org/10.55762/pc.gr.157042
Grantee: Rashmi Kothary, Ph.D.
Grant type: Research Grant
Award total: $300,000
Institution: Ottawa Hospital Research Institute
Country: Canada
Grantee: Neena Lala-Tabbert, Ph.D.
Funded: 9/1/2022 - 8/31/2025
Grant Type: Development Grant
Disease(s): Duchenne muscular dystrophy (DMD)

The NF-kB pathways form a signaling complex that is critical for normal skeletal muscle function and is important in promoting recovery in response to muscle injury. Furthermore, there is strong evidence that prolonged NF-kB activation is detrimental to normal skeletal muscle function and can contribute to diseases such as the common genetic disorder, Duchenne muscular dystrophy (DMD). As such, NF-kB has become an attractive drug target for the treatment of muscle diseases. It has been shown that cellular inhibitor of apoptosis 1, cIAP1, can modify NF-kB signaling in skeletal muscle in a beneficial manner. This discovery has raised the exciting possibility that cIAP1 may be a potential therapeutic target for various muscle diseases that are caused or worsened by prolonged NF-kB signaling. Since there are several drugs and reagents that potently and specifically eliminate cIAP1 expression, I will evaluate their therapeutic potential in mdx mice, the mouse model for DMD. I will also clarify the role that cIAP1 plays in the disordered muscle structure and function associated with DMD and how cIAP1 regulates NF-kB signaling in dystrophic muscle. Findings from this study have the potential to improve muscle structure and function and thus the quality of life of patients living with DMD.
Institution: Children's Hospital of Eastern Ontario Research Institute Inc
Institution Country: Canada
https://doi.org/10.55762/pc.gr.157031
Grantee: Neena Lala-Tabbert, Ph.D.
Grant type: Development Grant
Award total: $199,842.22
Institution: Children's Hospital of Eastern Ontario Research Institute Inc
Country: Canada
Grantee: Matthias Lambert
Funded: 9/1/2022 - 8/31/2025
Grant Type: Development Grant
Disease(s): Nemaline myopathies

TPM3-related myopathy is a muscular disorder caused by genetic defect in the tropomyosin-3 (TPM3) gene. Patients typically experience lifelong muscle weakness, eventually requiring the use of a wheelchair and nocturnal non-invasive ventilatory (NIV) support. So far, there is no treatment or cure for TPM3-related myopathy. Using the CRISPR-Cas9 genetic scissors, our lab developed mouse and zebrafish models of the disease that mirror the pathology seen in patients. In mouse, we aim to study the molecular events in muscle that contribute to the disease and to better drive the development of therapeutic strategies. Zebrafish also offers many advantages (small size, large number, rapid development ex utero, ability to absorb drugs) to complement studies in mouse. We aim to use the zebrafish as a straightforward and cost-effective platform to design targeted therapeutics using small compounds or mRNA strategies that reverse the pathology. Our long-term goal is to better understand the disease and provide efficient therapies for patients.
https://doi.org/10.55762/pc.gr.157029
Grantee: Matthias Lambert
Grant type: Development Grant
Award total: $210,000
Institution: Boston Children's Hospital
Country: Massachusetts, United States
Funded: 9/1/2022 - 8/31/2025
Grant Type: Research Grant
Disease(s): Duchenne muscular dystrophy (DMD)

Duchenne muscular dystrophy (DMD) is a fatal disease affecting around 1 in 3500 to 1 in 5000 live male births. Boys with DMD usually lose the ability to walk and feed in their teens, and die from respiratory insufficiency or cardiomyopathy in early adulthood. There is no cure for this disease at this time. In our previous studies, we found that a group muscle stem cells, named Fibro/adipogenic progenitors (FAPs) can differentiate into a brown fat-like cells to prevent muscle degeneration and promote muscle regeneration, under the stimulation of a group of drugs, called beta3 adrenergic receptor (B3AR) agonists. Mirabegron is a FDA approved B3AR agonist currently used for treating patients with hyperactive bladders, including kids. In our pilot study, we have shown that Mirabegron significantly improved the health and extended the life span of mice with DMD. In this study, we will determine the optimal dose of Mirabegron in treating DMD in a preclinical DMD mouse model. We will also define the role of Mirabegron in reducing heart and skeletal muscle fibrosis, a critical pathological change that leads heart failure and muscle weakness. Results from this study will provide essential preclinical data that allows the filing of clinical trials application of Mirabegron for treating DMD. Considering the fact that Mirabegron is a FDA approved drug, successful accomplishment of this study may lead to an expedite transition of clinical use of Mirabegron on DMD patients.
https://doi.org/10.55762/pc.gr.157014
Grantee: Xuhui Liu, MD
Grant type: Research Grant
Award total: $300,000
Institution: The Regents of the University of California, San Francisco
Country: United States
Grantee: Jocelyn Laporte, Ph.D.
Funded: 9/1/2022 - 8/31/2023
Disease(s): Distal myopathies

There is no therapy for the different caveolin(CAV3)-related muscle diseases that include distal myopathy with muscle weakness and atrophy, rippling muscle disease with myotonia, muscle cramps and pain, and idiopathic hyperCKemia with elevated blood creatine kinase (OMIM#614231, 606072, 123320). The primary cause of all these diseases are mutations in the protein caveolin 3 leading to alteration of the T-tubules, membrane tubes in the muscle fibers that allow coupling nerve excitation to muscle contraction. Here we propose to correct these T-tubules by increasing the level of another T-tubule protein called amphiphysin 2 (BIN1). Indeed, we recently showed BIN1 can correct T-tubule defect together with the phenotypes of two other myopathies, and we propose to now test this therapeutic approach for caveolin(CAV3)-related muscle diseases. We will use viral vectors and will test both whether this strategy can prevent disease progression and can revert established disease in a mouse model. This first proof-of-concept should trigger further preclinical development paving the way to clinical trials. Moreover, this strategy would represent a common approach to treat several muscle diseases while this project would extend the indications and thus promotes its translation to clinic.
https://doi.org/10.55762/pc.gr.157048
Grantee: Jocelyn Laporte, Ph.D.
Grant type: Idea Award
Award total: $50,000
Institution: Institute of Genetics and Molecular and Cellular Biology (IGBMC/CERBM)
Country: France