Dermatomyositis
Dermatomyositis
What is dermatomyositis?
 Dermatomyositis is one of the idiopathic inflammatory myopathies (IIMs), a group of muscle diseases that involves inflammation of the muscles or associated tissues, such as the blood vessels that supply the muscles. A myopathy is a muscle disease, and inflammation is response to cell damage. Another word for inflammatory myopathy is myositis. The myo root means muscle, and the itis root means inflammation; so a myositis is an inflammatory muscle disease.
Dermatomyositis is one of the idiopathic inflammatory myopathies (IIMs), a group of muscle diseases that involves inflammation of the muscles or associated tissues, such as the blood vessels that supply the muscles. A myopathy is a muscle disease, and inflammation is response to cell damage. Another word for inflammatory myopathy is myositis. The myo root means muscle, and the itis root means inflammation; so a myositis is an inflammatory muscle disease.
What are the symptoms of dermatomyositis?
Dermatomyositis is distinct among the muscle diseases for its manifestation in the skin (“dermato”). A reddish or purplish rash may occur over the face, neck and chest; on the shoulders and upper back, resembling a shawl; and/or on the elbows, knees and ankles. The skin may be scaly, dry and rough. Sometimes it looks like a sunburn.
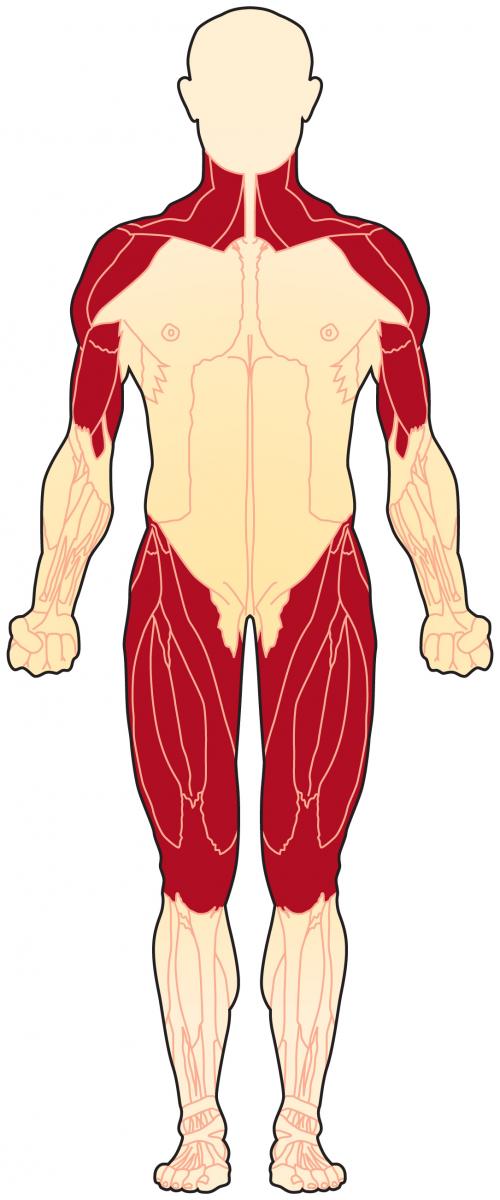
Over time, the inflammatory process in dermatomyositis leads to inflammation of muscle tissue, and is accompanied by weakness and sometimes pain. There can be loss of muscle bulk (atrophy). The muscles of the shoulders, upper arms, hips, thighs and neck display the most weakness in dermatomyositis. There also can be joint pain, inflammation of the heart and lung muscle tissues, as well as inflammation of blood vessels to other organs.
Other complications can also occur in dermatomyositis. For more, see Signs and Symptoms.
What causes dermatomyositis?
In most cases, the cause of an IIM is unclear. For some reason, the body’s immune system turns against its own muscles and damages muscle tissue in an autoimmune process. In dermatomyositis, these cells attack the small blood vessels that supply muscles and skin.
Dermatomyositis is not a genetic disorder, although there may be genetic factors that make it more or less likely that an inflammatory myopathy will develop. For more, see Causes/Inheritance.
What is the progression of dermatomyositis?
Onset of dermatomyositis occurs in adulthood, and its progression is gradual. In children, juvenile dermatomyositis (JDM) can occur, usually beginning between the ages of 5 and 14 and affecting girls more often than boys. Although inflammatory myopathies like dermatomyositis can lead to great discomfort for at least a period of time, effective treatments are available, and for the most part these conditions aren’t life-threatening. Dermatomyositis can, however, affect other organs besides the skin and muscle, leading to issues such as joint or lung inflammation. With treatment, many people recover partially or completely from dermatomyositis.
What is the status of research on dermatomyositis?
Research studies to increase the understanding of dermatomyositis and clinical trials of medications to treat IIMs are underway. For a list of dermatomyositis clinical trials, see MDA's Clinical Trials Finder Tool.
MDA educational resources
For patients and caregivers
For additional educational resources on neuromuscular disease, see mda.org/community-ed. New programs are posted periodically.
For healthcare professionals
- Myositis: Updates in Diagnosis & Treatment - CME-accredited webinar!
For additional clinical educational resources in neuromuscular disease, see mda.org/meded. New programs and resources are posted periodically. Sign up to receive updates via our Monthly Report for clinicians.
Additional resources
- MDA Resource Center
- MDA Resource List for Families
- MDA Research
- National Institute of Health: Inflammatory Myopathies
- Centers for Disease Control and Prevention: Muscular Dystrophy
- Outside Organization Programs & Information

